International bi-monthly journal of cell signaling, tissue protection, and translational research.
Using time-dependent intravenous infusions of amiodarone for conversion to sinus rhythm in patients with paroxysmal atrial fibrillation
Luis A. Sánchez-Trujillo1,2,3, Edgar Acuña-Morín1, José R. Azpiri4, Adán Pacheco- Cantú4, Leticia Elizondo-Montemayor1,3, Guillermo Torre-Amione1,3,5, Gerardo García-Rivas1,3
Author Affiliations


- 1Tecnologico de Monterrey. Escuela de Medicina y Ciencias de la Salud. Cátedra de Cardiología y Medicina Vascular. Monterrey. México
- 2Departamento de Cardiología. Unidad Médica de Alta Especialidad Hospital de Cardiología Num 34. Monterrey. Instituto Mexicano del Seguro Social. México
- 3Tecnologico de Monterrey. Centro de Investigación Biomédica. Hospital Zambrano-Hellion. San Pedro Garza-García. México
- 4Hospital Universitario “Dr. José Eleuterio González” and School of Medicine, Universidad Autónoma de Nuevo León, Monterrey, Mexico
- 5Houston Methodist DeBakey Heart & Vascular Center, Houston, Texas
Abstract
Background: Atrial fibrillation (AF), a well-known risk factor for cerebrovascular disease and heart failure, is the most common clinically significant arrhythmia worldwide. The management of emergency patients with newly diagnosed symptomatic AF is not completely standardized. Objective: Amiodarone infusions for 24 h and up to 72 h were compared—first, to determine patients’ rates of conversion to sinus rhythm, and second, to determine treatment related complications. Methods: Sixty patients with newly diagnosed AF in the emergency room were randomized into two groups of 30 subjects each. The first group received intravenous amiodarone infusion continuously for 24 h, and then oral amiodarone was continued for 24 h thereafter. The second group received the same infusion regimen for up to 72 h or shorter if sinus rhythm was achieved before. Results: Sinus rhythm conversion from AF occurred in 60% of all-subjects. Prolonged intravenous infusion of amiodarone increased cardioversion rates from 45% at 24 h to 60% at 48 h, with no further increase after 72 h. Complications occurred in 33% and 56.7% of the 24 h and 72 h groups respectively (risk ratio [RR] 2.6, 95% CI 0.91 to 7.4, p = 0.07). Conclusions: In newly diagnosed AF patients, prolonging the infusion regimen of intravenous amiodarone from 24 to 48 h increased rates of conversion to sinus rhythm, but after 72 hours there was no further increases. Furthermore, there was a 2.6 times increased risk of local complications with prolonged infusion.
Keywords: amidarone, atrial fibrillation, cardioconversion, complication, safety
Abstract
Background: Atrial fibrillation (AF), a well-known risk factor for cerebrovascular disease and heart failure, is the most common clinically significant arrhythmia worldwide. The management of emergency patients with newly diagnosed symptomatic AF is not completely standardized. Objective: Amiodarone infusions for 24 h and up to 72 h were compared—first, to determine patients’ rates of conversion to sinus rhythm, and second, to determine treatment related complications. Methods: Sixty patients with newly diagnosed AF in the emergency room were randomized into two groups of 30 subjects each. The first group received intravenous amiodarone infusion continuously for 24 h, and then oral amiodarone was continued for 24 h thereafter. The second group received the same infusion regimen for up to 72 h or shorter if sinus rhythm was achieved before. Results: Sinus rhythm conversion from AF occurred in 60% of all-subjects. Prolonged intravenous infusion of amiodarone increased cardioversion rates from 45% at 24 h to 60% at 48 h, with no further increase after 72 h. Complications occurred in 33% and 56.7% of the 24 h and 72 h groups respectively (risk ratio [RR] 2.6, 95% CI 0.91 to 7.4, p = 0.07). Conclusions: In newly diagnosed AF patients, prolonging the infusion regimen of intravenous amiodarone from 24 to 48 h increased rates of conversion to sinus rhythm, but after 72 hours there was no further increases. Furthermore, there was a 2.6 times increased risk of local complications with prolonged infusion.
Keywords: amidarone, atrial fibrillation, cardioconversion, complication, safety
Introduction
Atrial fibrillation (AF) is the most common clinically significant arrhythmia worldwide. AF is responsible for one third of all hospital admissions for arrhythmia (Cotter et al., 1999; Thomas et al., 2004; Fuster et al., 2006). Its prevalence increases from 1%-3% in individuals over 60 years of age to 7%-13% in individuals over the age of 80 in the United States (Go et al., 2001). Moreover, symptoms can have significant impact on a patient’s functional status, quality of life, and cardiovascular function (Snow et al., 2003). AF increases the risk of brain thromboembolism by five-fold and the risk of mortality by two-fold compared with the general population (Benjamin et al., 1998; Cotter et al., 1999; Waldo, 1999; Go et al., 2001; Joseph et al., 2001; Wyse et al., 2002; Snow et al., 2003; Tuseth et al., 2005; Fuster et al., 2006), independently of underlying cardiovascular disease (Fuster et al., 2006). Indeed, AF is considered a cardiovascular pandemic among the aging population. In addition to this fact, it has become a public health problem due to its increased incidence and prevalence (Carlsson et al., 2003).
Several studies have assessed different treatment strategies for paroxysmal AF. Pharmacological rhythm control and heart rate management are the two widely accepted strategies. However, there are knowledge gaps regarding optimal treatments protocols for patients with first symptomatic episodes of AF (i.e., with episodes that lasted less than 48 h). Electrical cardioversion is considered the first choice when hemodynamic instability is present (class IB recommendation), but pharmacological cardioversion has proven to be highly effective in all other groups of patients (Chevalier et al., 2003; Del Arco et al., 2005; Decker et al., 2008; January et al., 2014; ( National Institute of Health and Clinical Excellence, 2014).
Restoration to sinus rhythms is often attempted for acute events with the goals being to decrease patients’ symptoms, reduce patients’ risks of cerebral thromboembolisms, and prevent the development of heart failure. Antiarrhythmic drugs for acute restoration restore sinus rhythm in approximately 50% of patients with recent-onset AF, with current guidelines recommending amiodarone combined with a class IA antiarrhythmic drug (Waldo, 1999; Carlsson et al., 2003). However, this combined strategy is not always successful in clinical practice. Thus, the objective of the current study was to evaluate the efficacy of AF rhythm conversion induced by prolonged administration of amiodarone (up to 72 h), and to determine the complications of such a strategy compared to a standard 24 h infusion of amiodarone followed by oral amiodarone. No appropriate therapeutic regimen for amiodarone infusion has been defined for AF, with a delayed effect frequently observed. There is currently no way to assess the effectiveness of a prolonged infusion strategy on improving the rate of conversion to sinus rhythm without altering the safety profile of the drug.
Materials and Methods
This study was approved by the institutional ethics committee at Hospital Universitario, Universidad Autónoma de Nuevo León, and registered at Clinicaltrial.gov (NTC00345592). The study was an open-label randomized clinical trial comprising 60 adult patients who presented to the emergency room, and who were candidates for pharmacological cardioversion after the first symptomatic episode of AF. The patients were ≥ 18 years of age who agreed to participate and gave written informed consent. Exclusion criteria for the study were hemodynamic instability requiring electrical cardioversion, the previous use of antiarrhythmic drugs, and the use of digoxin in the past seven days prior to the study. Additionally, patients with active thyroid disease, known adverse reactions to amiodarone, other ventricular arrhythmias, contraindications for anticoagulation, acute renal failure, chronic liver disease, transaminase levels that were twice the normal levels, acute pulmonary edemas, uncontrolled hypertension (> 180/110 mmHg) and/or unstable angina were excluded, as well as patients who were pregnant and/or breast feeding.
Patients were randomized through an allocation system by the research committee. The doctors and nurse were aware of the group to which the patient belonged, but the patients/subjects were not aware of their group assignment. Adverse outcomes were assessed by the medical team. The two groups received intravenous amiodarone infusion at doses of 5 mg/kg for 30 min followed by 20 mg/kg for up to 24 h. The 24 h group continued with oral amiodarone, while the 72 h group continued to receive 20 mg/kg infusion of amiodarone every 24 h for up to 72 h. Both groups were subjected to continuous electrocardiographic monitoring. Patient death, discontinuation of the infusion for reasons other than adverse effects of amiodarone, and the discovery that a patient had previously undiagnosed thyroid disease were considered as withdrawal criteria.
An echocardiogram was performed within 24 h after randomization into treatment groups. The echo protocol included structural and functional parameter previously described as prognostic of AF cardioversion, particularly left atrium and ventricle dimensions, ventricular function, and thrombus search. The exact time of each patient’s cardioversion was documented. In addition, lipid profiles, thyroid profiles, cardiac biomarker at admission and every 24 hours thereafter, as well as other blood tests, were carried out at the discretion of the attending physician.
Statistical analysis
The data’s distribution was determined and statistical tests were selected accordingly. Continuous variables were expressed as mean ± standard deviation, and their differences were tested using Student’s t test. Nominal variables were expressed as frequencies, and their differences were tested using the chi-square test, or Fisher’s test. The primary and secondary endpoints (i.e., the conversion and complication rates) were expressed as frequencies and relative risks (RR) with 95% CI. The relationships between diverse variables of conversion to sinus rhythms and medical treatments were estimated using univariate regressions. Afterwards, significant variables were incorporated into Cox multivariate regression analysis. A difference was considered significant when a p value was less than 0.05.
Results
A total of 122 subjects with newly diagnosed AF were evaluated in a 16-month period. From these, 69 were eligible for the study and randomly allocated into one of the two groups, as shown in Figure 1. A total of nine subjects were withdrawn for reasons previously mentioned as exclusion criteria, and 53 subjects were excluded primarily because of hemodynamic instability, acute myocardial infarction, previous antiarrhythmic drug use, or active thyroid disease.
In a new window | Download PPT
Figure 1: Flow diagram for inclusion/exclusion/elimination of patients in the randomized study.
Each group finally consisted of 30 randomized subjects. The baseline clinical characteristics of each group are summarized in Table 1. The patients’ mean (± standard deviation) age was 63 years old ± 15 years (women = 33 (55%)). More patients in the 24 h group had chest pain as a chief complaint than patients in the 72 h group: 22 (73%) and 14 (46%) complained of chest pain, respectively (p = 0.03). In contrast, 26% of patients in the 72 h group presented with syncope while only 13% of patients in the 24 h group presented with syncope (p = 0.19). Additionally, in the 72 h group, 83% of the subjects presented with left atrium diameter greater than 45 mm whereas in the 24 h group, only 60% of the subjects had a left atrium diameter of greater than 45 mm (p = 0.04).
Table 1. Baseline characteristics.
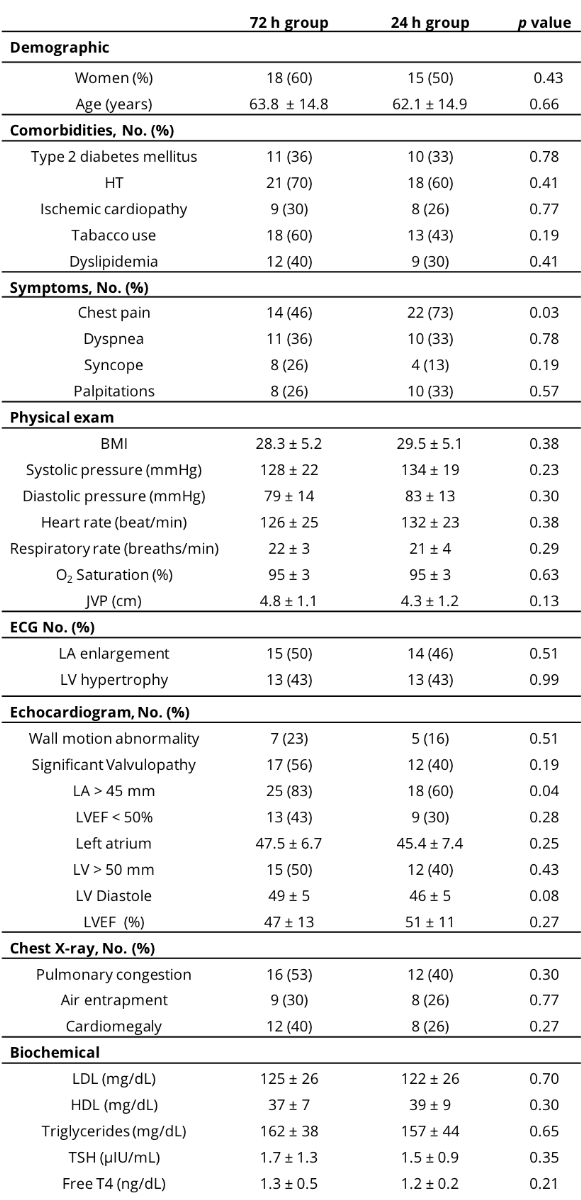
HT = hypertension; BMI = body mass index; JVP = jugular venous pressure; LA = left atrium; LV left ventricle; LVEF = left ventricular ejection fraction; TSH = thyroid stimulating hormone; T4 = tetraiodothyronine.
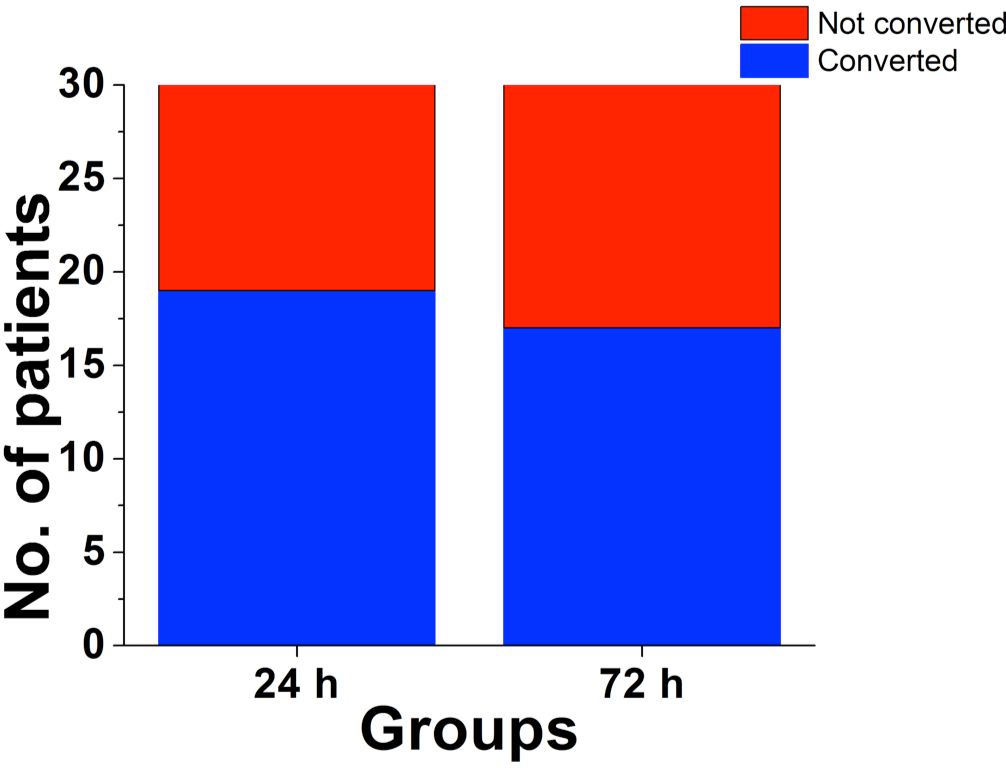
The overall conversion rate, which was the primary endpoint, was reached in 60% of the subjects. At the end of the 72 h, the conversion rate was achieved in 19 subjects (63.3%) in the 24 h group and in 17 subjects (56.7%) in the 72 h group. The average time for a conversion to sinus rhythm, for the total sample, was 22 h ± 2.2 h (Figure 2).
In a new window | Download PPT
Figure 2: The rate of cardioconversion to sinus rhythm in the 24 and 72 h. groups.
The mean conversion time was 14.8 h ± 5.1 h for the 24 h group and 27.5 h ± 11.3 h for the 72 h group (p < 0.0001). At the 24 h point, the conversion rate was 63.3% for the 24 h group and 30% for the 72 h group. Conversion to sinus rhythms within 24 h was achieved in 30% of the patients in the 72 h group. Therefore, intravenous infusion was discontinued and patients were given oral amiodarone instead. Eight patients converted to sinus rhythms between 24 and 48 h after initiation of therapy. None of the 13 (43.3%) patients in the 72 h group who continued with infusions beyond 48 h converted to sinus rhythms. The conversion rate of the total sample, continued to increase for up to 48 h; but there was no further increase thereafter. The secondary endpoint occurred in 27 subjects (45%). Specifically, it was achieved for 33% of the subjects in the 24 h group and 56.7% of the subjects in the 72 h group. The relative risk of complications was 2.6, with a 95% CI of 0.91–7.4 (p = 0.07). No statistically significant differences between the groups were observed. Specific complications that were observed are shown in Table 2.
Table 2. Adverse events according to randomization.
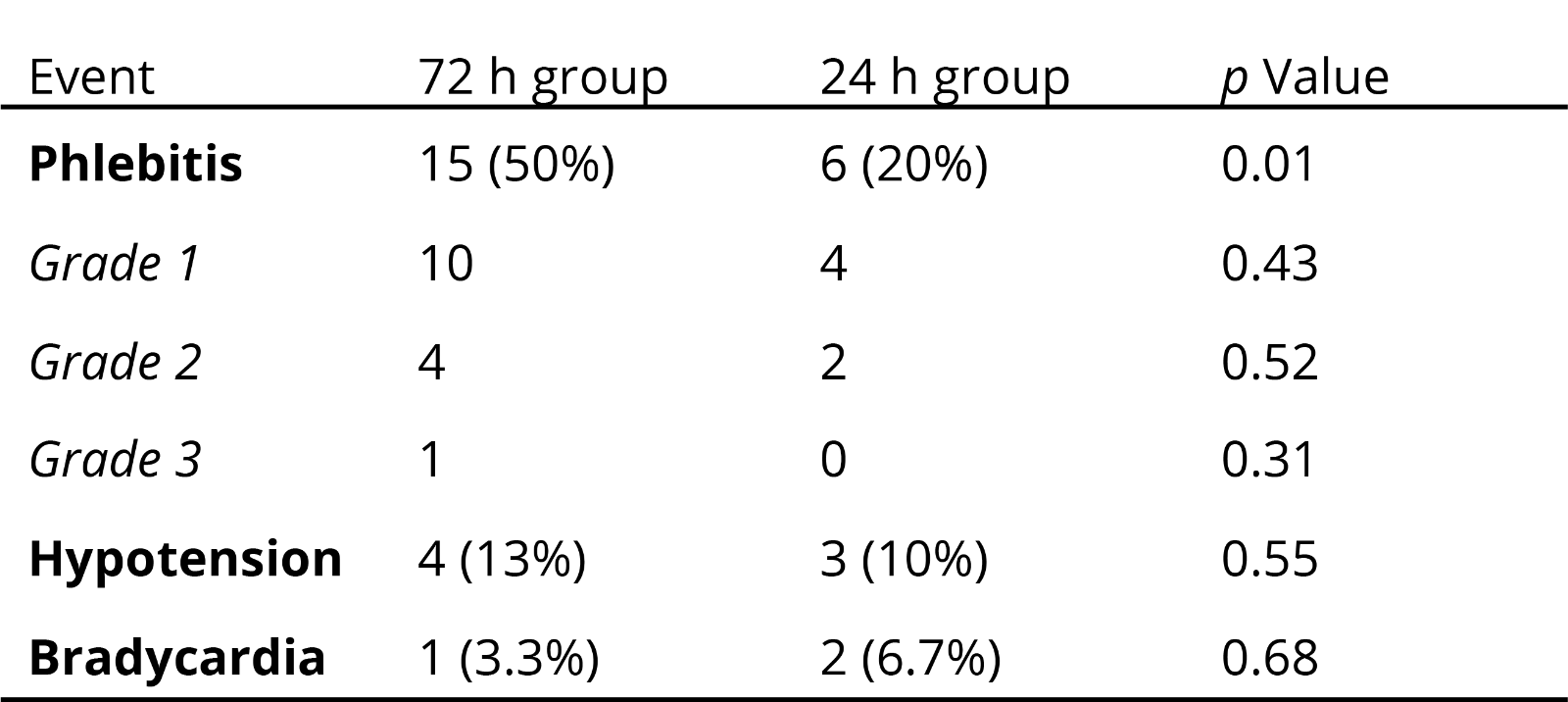
The adverse effects observed were not severe. Phlebitis appeared in 35% of the total population, which accounted for 84% of all complications. Divided by groups, phlebitis was presented by 20% of the subjects in the 24 h group and in 50% of the subjects in the 72 h group (p = 0.01). Several factors were identified as independent negative predictors of conversion to sinus rhythms (Table 3), such as jugular venous pressure or congestive heart failure, which remained significant after adjustments for age, gender and left-atrium size.
Table 3. Predictive factors for non-cardioverison to sinus rhythm.
.png)
Discussion
To our knowledge this is the first randomized study that compares two different antiarrhythmic schemes of prolonged intravenous amiodarone infusion. The study showed that prolonging infusions of amiodarone beyond the 24 h traditional treatment period in patients who do not convert to sinus rhythms within this time frame, increased cardioversion rates in patients at 48 hours. However, prolonged treatment resulted in a significant increase in the complication rates at 72 h. Considering a conversion rate of 45% for both groups at 24 h and an increase to 60% if patients continued infusions for an additional 24 h, an absolute increase in conversion rate of 15% was observed at 48 h. These data suggest that some patients who present with AF may benefit from prolonged infusions. This result may be used to clarify guidelines that only recommend using infusions for shorter times due to a lack of data (January et al., 2014).
The low rate of cardioversion at 24 h that was found in this study is comparable to a low rate reported by Kreiss et al., (1999) who used a dose of amiodarone similar to our study’s initial 24 h dose. However, our study’s cardioversion rate is lower than cardioversion rates found in other studies, such as a study by Cotter et al., (1999), which reported a conversion rate of 92% with the same dose of amiodarone. Another study reported that a high dose of oral amiodarone resulted in conversions to sinus rhythms in fewer than 24 h (Nadarasa et al., 2012). However, in the current study patients who previously used antiarrhythmic drugs, such as digoxin and beta-blockers were excluded. Furthermore, to isolate the effects of amiodarone, the use of additional antiarrhythmic drugs was not allowed. This might partly explain the low rate of cardioversion in the current study, in addition to clinical and echocardiographic characteristics previously described (Wyse et al., 2002).
None of the patients in the current study who received amiodarone, intravenously or orally, beyond 48 h achieved sinus rhythm. Therefore, it was not possible to demonstrate clearly the benefits of amiodarone use beyond that time point. Most patients who converted to sinus rhythms did so within 24 h, and only eight randomized patients in the 72 h group did so between 24 h and 48 h. It is notable that the randomized patients in the 72 h group converted to sinus rhythms at an average of 27.5 h ± 11.3 h, while the randomized patients in the 24 h group converted to sinus rhythms at an average of 14.8 h ± 5.1 h. This difference might be explained by the differences in baseline characteristics of the patients in the 72 h group, despite the randomization. Compared to the 24 h group, the patients in the 72 h group were older, had greater body mass indices, had a greater number of comorbidities (especially hypertensive cardiomyopathy), and presented with syncope more often. This may indicate that more patients in the 72 h group were in advanced stages of generalized atherosclerosis. Notably, left atria that were bigger than 45 mm diameter were present in 83% of the subjects in the 72 h group but present in only 60% of the subjects in the 24 h group. It is possible that these and other non-identified factors influenced the 72 h group’s slower and less frequent responses to amiodarone infusions, as these data are known to be risk factors of non-conversion to sinus rhythm (Danias et al., 1998; Patel et al., 2009; Emren et al., 2016; Suenari et al., 2017). However, these unknown factors could be identified in further studies. As aforementioned, an increase in the combined complication rate of the 72 h group was observed, although this was not statistically significant. A feasible explanation is the use of small-caliber peripheral catheters and distal placement in the limbs (hands or forearms) of the patients. Additionally, the intravenous route was not used exclusively for amiodarone administration. This factor was not controlled during the study, as is common practice. On the other hand, the doses and dilutions used in this study were similar to the doses and dilutions used in other studies in which phlebitis rates of 25% were reported (Cotter et al., 1999; Snow et al., 2003). However, amiodarone was not infused for more than 24 h in other studies. Although some studies reported severe adverse effects of prolonged amiodarone use (Freemantle et al., 2011), most of the adverse effects noted in this study were minor, and almost all were noted in the 72 h group. Phlebitis that was mild and reversible, and for which patients presented few symptoms was noted in 35% of the group. Nausea was noted in 33% of the group and vomiting was noted in 13% of the group.
This study considered the possibility of developing new therapeutic schemes with known available antiarrhythmic drugs, such as amiodarone, in order to improve patients’ cardioversion rates without increasing patients’ risks of major complications. In doing so, it introduced the possibility of improving the risk profiles of patients who do not cardiovert within 24 h. This potential improvement in risk profiles is particularly important for patients in locations where electrical cardioversion is not used routinely (Vardas et al., 2000). Moreover, this study was the first to evaluate the effects of administering amiodarone infusions beyond 48 h for newly onset AF. Actual guidelines only consider amiodarone infusions for 18 h (January et al., 2014).
Our study has some limitations, such as a small and heterogeneous sample. The sample size did not allow the application of the study’s results to other populations, and it limited the researchers’ ability to determine risks of acute thromboembolisms and other major complications. Additionally, infusions were discontinued for the 72 h group when subjects converted to sinus rhythms; then, amiodarone was administered orally. This possibly caused the accumulative effects of amiodarone to be underestimated. Moreover, there was no follow up with patients to assess the maintenance of their sinus rhythms after their infusions were discontinued. Furthermore, serum concentrations of amiodarone were not measured in this study, because such measurements are not routinely conducted as they do not correlate with amiodarone efficacy (Xanthos et al., 2007).
Conclusions
Prolonged infusions of amiodarone increase patients’ cardioversion rates from 45%–60% for up to 48 h (i.e., it results in an absolute increase of 15%). Moreover, while increasing infusions for more than 48 h does not increase conversion rates, it can increase incidences of local complications.
Our study suggests that an infusion of amiodarone might be considered for up to 48 hours in stable patients with a low risk of local complications when other therapeutic options are not available or are contraindicated, considering the factors that predict a successful cardioversion. New schemes should be sought to minimize the incidence of adverse effects and favor early cardioversion with antiarrhythmics.
Disclosures/conflicts
The authors declare that they have no conflicts of interest.
Acknowledgements
This work was partially supported by Endowed Chair in Cardiology /Grupo de Enfoque Medicina Molecular- Tec de Monterrey and CONACYT grants CB-256577 (G. García-Rivas).
References
Luis A. Sánchez-Trujillo1,2,3
Corresponse should be addressed to
Luis A. Sánchez-Trujillo
Email: gdejesus@itesm.mx
In a new window | Download PPT
Figure 1: Flow diagram for inclusion/exclusion/elimination of patients in the randomized study.
In a new window | Download PPT
Figure 2: The rate of cardioconversion to sinus rhythm in the 24 and 72 h. groups.
Table 1. Baseline characteristics.
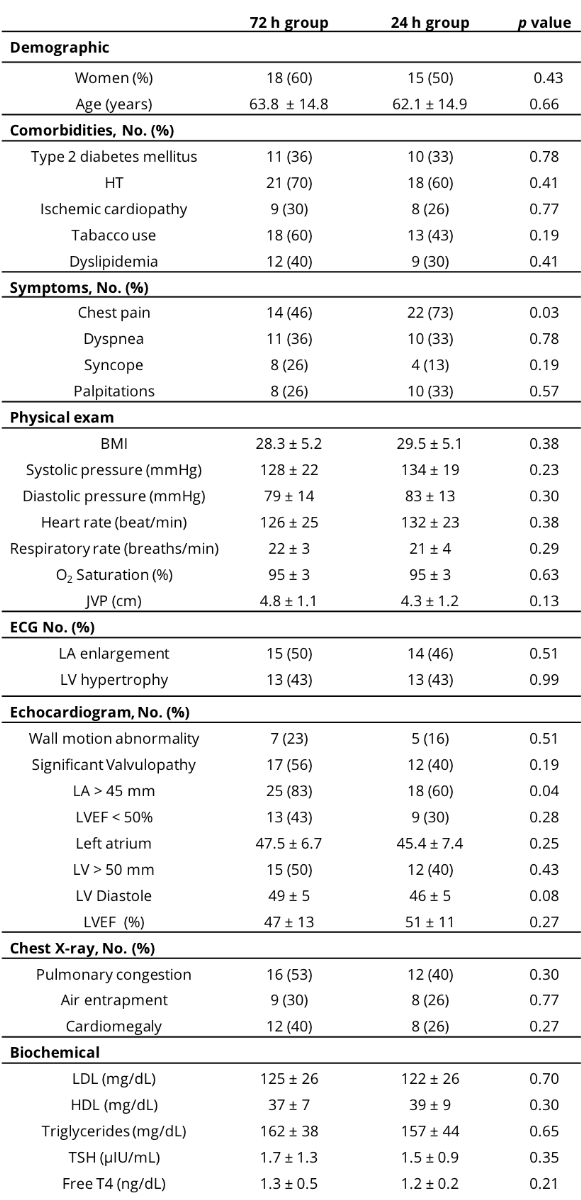
HT = hypertension; BMI = body mass index; JVP = jugular venous pressure; LA = left atrium; LV left ventricle; LVEF = left ventricular ejection fraction; TSH = thyroid stimulating hormone; T4 = tetraiodothyronine.
Table 2. Adverse events according to randomization.
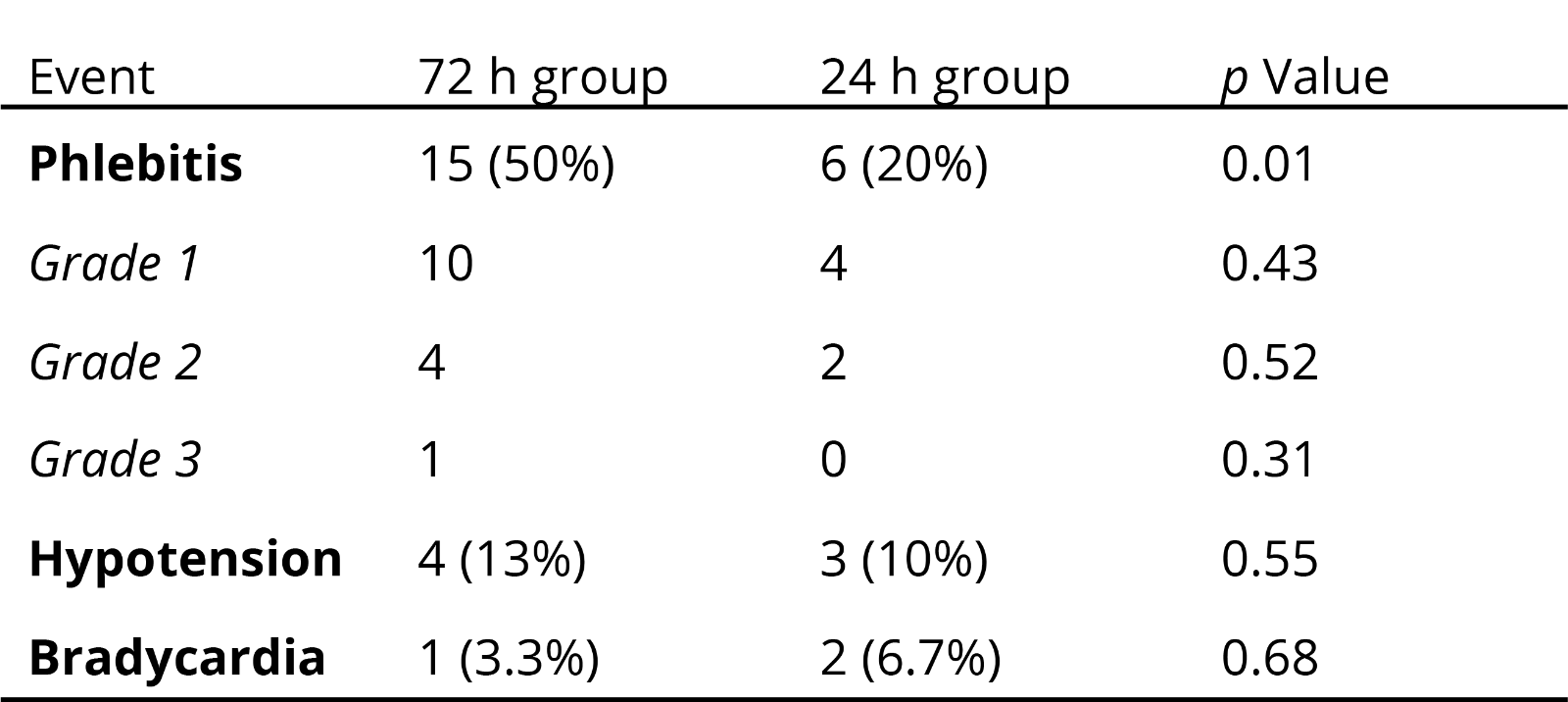
Table 3. Predictive factors for non-cardioverison to sinus rhythm.
.png)
Supporting Information
Metrics
| Full-Text | Supporting Information | ||
|---|---|---|---|
| Number | 11214 | 24 | 0 |
Copyright © 2017 Conditioning Medicine, All Rights Reserved.
Address: Conditioning Medicine Editorial Office, 3500 Terrace Street, Pittsburgh, PA, 15213, USA