Browse Articles
Conditioning Medicine
International bi-monthly journal of cell signaling, tissue protection, and translational research.
Current Location:Home / Browse Articles
Clinical outcomes a decade following percutaneous coronary intervention or coronary artery bypass grafting surgery: insights from randomized controlled trials
Time:2022-10-15
Number:4643
Timothy Woodhead1, Connor Jack Matthews1, Heerajnarain Bulluck1,2
Author Affiliations


- 1Yorkshire Heart Centre, Leeds General Infirmary, Leeds Teaching Hospitals NHS Trust, Leeds, UK.
- 2Leeds Institute of Cardiovascular and Metabolic Medicine, University of Leeds, Leeds, UK.
Conditioning Medicine 2022. 5(3): 100-104.
Abstract
Coronary artery disease (CAD) is a leading cause of morbidity and mortality worldwide and treatment of CAD in the modern era involves a combination of optimized medical therapy, with or without revascularization with percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG). A limited number of randomized controlled trials (RCTs) have recently reported 10-year outcome following PCI or CABG in patients with predominantly stable CAD and this review aims to appraise the current literature and provide an overview of where we stand in terms of long-term morbidity and mortality between PCI and CABG in patients with left main stem (LMS) or multi-vessel CAD. The current data would suggest no mortality benefit at 10 years between PCI and CABG. However, PCI is associated with a 2-fold increased risk of repeat revascularization at 10 years. Diabetic status and coronary disease complexity do not seem to impact on 10-year mortality but do impact on repeat revascularization. In cases when the heart team considers either PCI or CABG to be equipoise after assessing the anatomical and clinical factors for each patient and depending on local level of expertise to perform complex revascularization, involving the individual patients in the decision-making process may help to offer them the optimal treatment. Longer term outcomes from existing studies are eagerly awaited to strengthen the evidence between PCI and CABG and the interaction between disease location, diabetes status and CAD complexity.
Keywords: Percutaneous coronary intervention, Coronary artery bypass grafting surgery, Mortality; Left main stem disease, Multi-vessel disease
Abstract
Coronary artery disease (CAD) is a leading cause of morbidity and mortality worldwide and treatment of CAD in the modern era involves a combination of optimized medical therapy, with or without revascularization with percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG). A limited number of randomized controlled trials (RCTs) have recently reported 10-year outcome following PCI or CABG in patients with predominantly stable CAD and this review aims to appraise the current literature and provide an overview of where we stand in terms of long-term morbidity and mortality between PCI and CABG in patients with left main stem (LMS) or multi-vessel CAD. The current data would suggest no mortality benefit at 10 years between PCI and CABG. However, PCI is associated with a 2-fold increased risk of repeat revascularization at 10 years. Diabetic status and coronary disease complexity do not seem to impact on 10-year mortality but do impact on repeat revascularization. In cases when the heart team considers either PCI or CABG to be equipoise after assessing the anatomical and clinical factors for each patient and depending on local level of expertise to perform complex revascularization, involving the individual patients in the decision-making process may help to offer them the optimal treatment. Longer term outcomes from existing studies are eagerly awaited to strengthen the evidence between PCI and CABG and the interaction between disease location, diabetes status and CAD complexity.
Keywords: Percutaneous coronary intervention, Coronary artery bypass grafting surgery, Mortality; Left main stem disease, Multi-vessel disease
Introduction
Coronary artery disease (CAD) is a leading cause of morbidity and mortality worldwide (Nowbar et al., 2019). Evidence-based treatment of CAD in the modern era involves a combination of optimized medical therapy with or without revascularization with percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) (Neumann et al., 2018; Lawton et al., 2022). However, the optimal choice for an individual patient remains a subject of discussion.
CABG surgery was initially performed in the late 1960s (Green et al., 1968). Survival has consistently been shown to be superior to contemporary medical therapies (Windecker et al., 2014), leading to mainstream uptake and worldwide popularization. Development of minimally invasive techniques (Robinson et al., 1995) have enhanced outcomes further. As such, one can regard CABG as the ‘gold-standard’ of revascularization. However, given the stress that cardiac surgery exerts upon the patient, it is not a universal option and suitability is determined by a multidisciplinary approach (Head et al., 2013), considering pre-operative risk, disease complexity, and patient choice. Furthermore, studies have shown benefit only in a subset of patients with multivessel coronary disease or left main stem (LMS) CAD (Windecker et al., 2014). These are regarded as well-defined indications for consideration of CABG (Neumann et al., 2018; Lawton et al., 2022).
The advent of percutaneous coronary intervention (PCI) for CAD in the 1970s in the form of balloon angioplasty provided a less invasive option in management of ischemic heart disease (IHD) (Grüntzig, 1978). Coronary angiography allows both diagnosis and simultaneous treatment of coronary lesions. This is of particular value in the setting of acute coronary syndrome where flow-limiting lesions can be addressed in the acutely unstable patient (Collet et al., 2021). Initially high levels of restenosis were seen with bare-metal stents (BMS) (Brophy et al., 2003) and the introduction of drug-eluting stents (DES) have greatly reduced rates of restenosis (Morice et al., 2007). Improvement in technologies such as thinner strut stents, fractional flow reserve (FFR), and the availability of intravascular imaging have broadened the range of applications for PCI, pushing it to the forefront of IHD management.
The obvious comparison between this “novel” method of revascularization and the relatively established method of CABG was inevitable. A few randomized controlled trials (RCTs) (Buszman et al., 2016; Thuijs et al., 2019; Park et al., 2020) have recently reported 10-year outcome following PCI or CABG in patients with predominantly stable CAD and this review aims to appraise the current literature and provide an overview of the status quo in terms of long-term (minimum of 10 years) morbidity and mortality between PCI and CABG in patients with LMS or multi-vessel CAD.
Methods
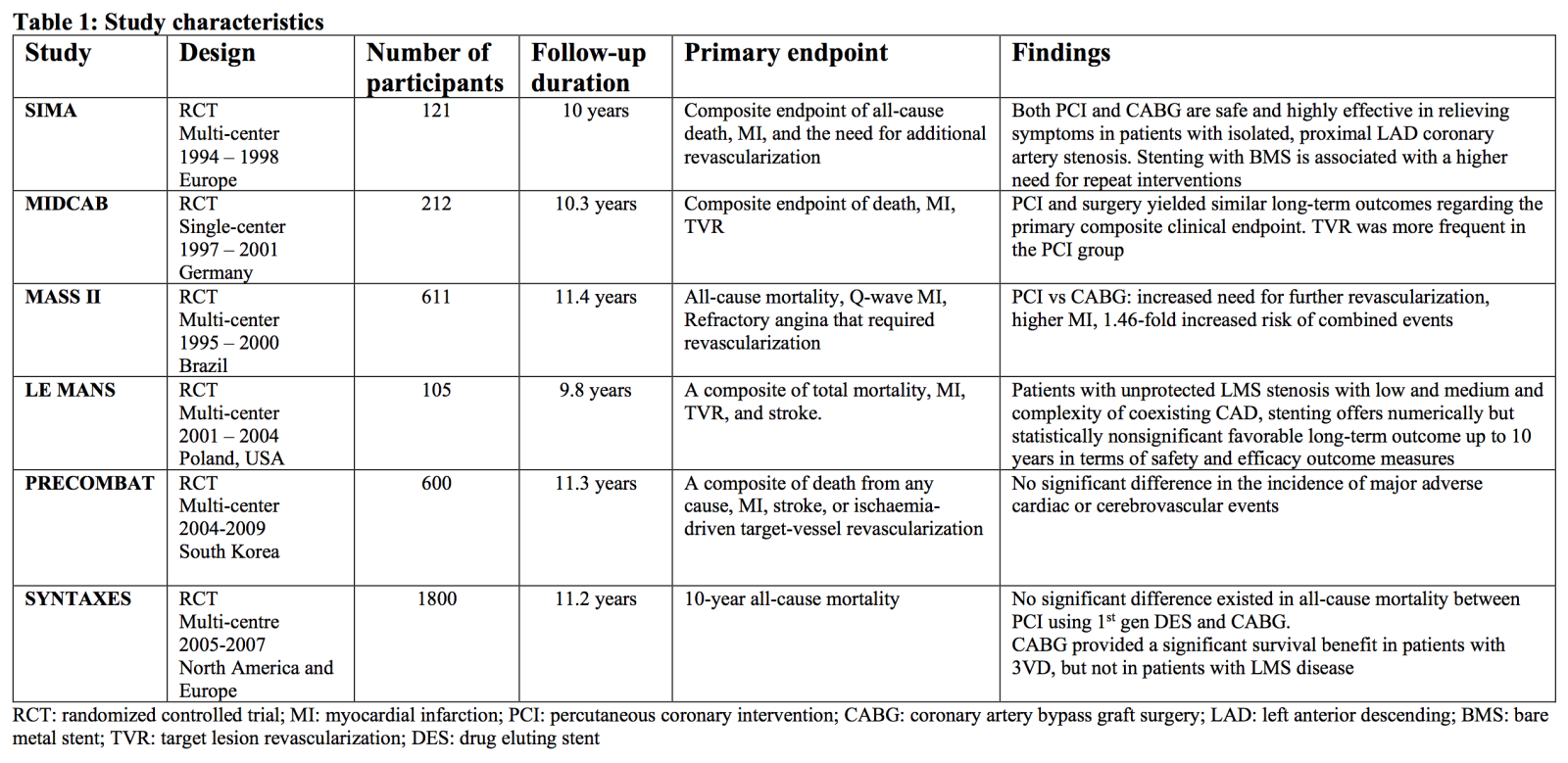
For this mini-review, we searched the Medline and Embase databases from inception through to May 2022. Only RCTs comparing PCI against CABG and reporting a minimum of 10-year outcomes were included in this review (Table 1). Studies reporting less than 10 years follow-up or observational studies were not included in this review.
10-year outcome following PCI or CABG in isolated proximal LAD disease
The SIMA (Stenting versus Internal Mammary Artery grafting) trial was a small multi-centre RCT comparing PCI with BMS versus CABG in patients with isolated proximal left anterior descending (LAD) coronary artery stenosis in 121 patients (Goy et al., 2008). The composite endpoint of all-cause death, myocardial infarction (MI) and repeat revascularization was significantly higher in the PCI arm (42%) when compared to the CABG arm (17%), and this was mainly driven by repeat revascularization (15% versus 0%, P<0.001). However, there was no difference in death or MI. This study was not adequately powered for these hard clinical endpoints and the patients in the PCI arm were treated with first generation BMS.
The MIDCAB (Minimally Invasive Direct Coronary Artery Bypass surgery) trial (Blazek et al., 2013) randomized 212 patients with isolated proximal LAD stenosis to either PCI or CABG (MIDCAB). At 10-years, there was no significant difference in the composite endpoint of all-cause death, MI, or target vessel revascularization (TVR) (47% versus 36%, P = 0.12). However, the rate of TVR was 34% in the PCI arm versus 11% in the CABG arm, and the difference was statistically significant (P < 0.01). Of note, similar to the SIMA trial, BMS was the stent used in the MIDCAB trial and this could explain the higher TVR at 10 years. Of note, the rate of TVR with DES was improved significantly when compared with BMS (Brugaletta et al., 2021).
10-year outcome following PCI or CABG in non-LMS multi-vessel and LMS disease
One of the earlier RCTs to compare PCI, CABG, and medical therapy was the MASS II (Medicine, Angioplasty, or Surgery Study) (Hueb et al., 2010). It remains one of the few studies to publish 10-year outcomes on its cohort of 611 patients with 2 or 3 vessel non-LMS CAD randomized to PCI (with either balloon angioplasty alone or BMS), CABG, or medical therapy (in line with best available evidence at the time). Ten-year follow-up was concluded in 2010, showing significantly superior outcomes for both CABG and PCI over medical therapy. For a primary composite endpoint of mortality, Q-wave MI and repeat revascularization, a higher event rate was seen in the PCI group versus the CABG group (multivariate hazard ratio (HR) 1.46, 95% CI 1.06-2.02). This was driven by a higher rate of acute MI (HR 2.09, 95% CI 1.39-6.01) and repeat revascularization (HR 3.71, 95% CI 1.82-7.52); no difference in overall mortality was seen (HR 1.34, 95% CI 0.77-2.34). As only a minority of patients received PCI with stents, this study does not reflect current practice and was underpowered for 10-year outcomes.
The LE MANS (Left Main Stenting) trial (Buszman et al., 2016) enrolled 105 patients with unprotected LMS CAD and low to medium coronary anatomical complexity and randomized to PCI with either BMS (35%) or DES (65%), or CABG. At 10-year follow-up there was no significant difference in overall mortality, major adverse cardiac and cerebrovascular event (MACCE), stroke, MI or repeat revascularization. At 14-year follow-up no difference was seen in overall mortality rate, however the rate of MACCE-free survival was numerically higher in the PCI group but was not statistically significant (PCI 34.7% versus CABG 22.1%; HR 1.71, 95% CI 0.97-2.99). Of note, this was a small study and was underpowered for 10-year outcomes.
An extended follow-up of the PRECOMBAT (Premier of Randomized Comparison of Bypass Surgery versus Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease) trial (Park et al., 2020) has recently been published reporting 10-year outcomes for their initial RCT. The recruited 600 patients with de novo stenosis of the left main coronary artery were randomized to receive either PCI with first generation DES or CABG with median 11.3 years follow-up (IQR 10.2-13.0). Ten-year data were acquired for 576 of the original 600 patient cohort. The stated primary outcome was a composite endpoint of MACCE at 10 years; no statistically significant difference was seen between the groups (PCI 29.8% versus CABG 24.7%; HR 1.25, 95% CI 0.93-1.69). All-cause mortality was similarly non-significant (PCI 14.5% versus CABG 13.8%; HR 1.13, 95% CI 0.75-1.70), with the only significant finding reported being any revascularization, occurring more frequently in the PCI group (PCI 21.3% versus CABG 10.6%; HR 2.04, 95% CI 1.33-3.11). The authors noted the significant contribution of revascularization to the composite endpoint and a high crossover rate between the groups as limitations of the conclusions.
In 2020, the SYNTAXES (Synergy between PCI with Taxus and Cardiac Surgery Extended Survival) trial (Thuijs et al., 2019) concluded 10-year follow up of 1800 patients randomized to either PCI with first generation DES or CABG. They reported no significant difference in overall mortality between the arms at 10 years (PCI 28% versus CABG 24%; HR 1·19, 95% CI 0·99–1·43, p = 0·066). When stratifying patients by whether they had multivessel disease involving the LMS or not, the mortality rate was significantly higher in the non-LMS subgroup for those undergoing PCI (PCI 28% versus CABG 21%; HR 1·42 (95% CI 1·11–1·81)) versus the LMS subgroup (PCI 27% versus CABG 28%; HR 0·92 (95% CI 0·69–1·22). Further subgroup analyses showed no significant interaction with SYNTAX score or diabetes status, although a SYNTAX score >33 was associated with higher mortality in the PCI group (HR 1.47 (95% CI 1.10-1.96) and the authors noted a visual trend towards favoring CABG as SYNTAX score increased. The lack of interaction with diabetes status was postulated to be likely due a small sample size (n = 452).
The above RCTs individually were not powered for 10-year mortality. A recent meta-analysis by Woodhead et al (2022) included the above 4 RCTs with a total of 2913 participants (SYNTAXES, PRECOMBAT, LE MANS, MASS II), specifically looking at 10-year mortality for PCI vs CABG. They concluded that there was no overall mortality benefit (RR 1.05, 95% CI 0.86-1.28) when considering the pooled cohort, and no significant difference when 10-year mortality was stratified by LMS (RR 0.94, 95% CI 0.78 to 1.15) or non-LMS (RR 1.16, 95% CI 0.83-1.63) multivessel disease. The authors concluded no significant mortality benefit from revascularization strategy regardless of disease location at 10 years. However, the included RCTs were heterogenous, spanning the pre-stent, BMS and DES eras. Nevertheless, this work provides some reassurance that despite the use of balloon angioplasty and older generations BMS and DES, there was no survival advantage of CABG over PCI at 10 years.
Discussion
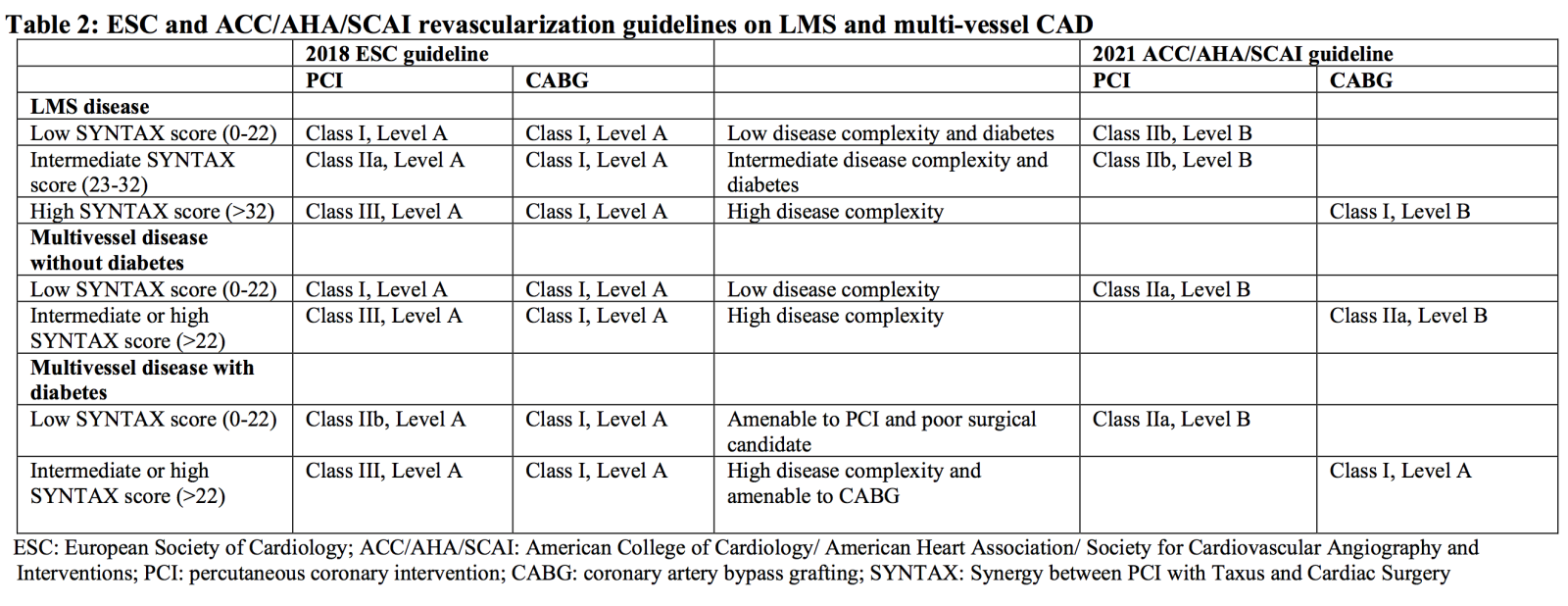
Current European society of Cardiology (ESC) (Neumann et al., 2018) and American College of Cardiology (ACC)/ American Heart Association (AHA)/ Society for Cardiovascular Angiography and Interventions (SCAI) (Lawton et al., 2022) guidelines advocate a “Heart Team” multidisciplinary approach for the management of IHD, due to inter-center variation in CABG-PCI rates. Certain factors may preclude choice of one approach e.g. surgical risk or anatomical suitability, thereby making the decision more straightforward. In the remainder, factors with a modifying effect identified in these guidelines include primarily disease location (non-LMS multivessel disease versus LMS), diabetes status and coronary anatomical complexity (Synergy between PCI with Taxus and Cardiac Surgery (SYNTAX) score (Sianos et al., 2005): low ≤22, intermediate 23-32, high ≥33) as summarized in Table 2. Of note, the 2018 ESC guideline (Neumann et al., 2018) was published prior to the SYNTAXES and PRECOMBAT 10-year follow-up results. The 2021 ACC/AHA/SCAI guideline (Lawton et al., 2022) has since downgraded recommendations for CABG to a Class I to improve survival only allocated to either 3-vessel disease in the setting of systolic dysfunction (left ventricular ejection fraction <35%) or severe LMS disease. For those with 3-vessel disease with preserved systolic function, CABG now has a Class IIb recommendation when compared to a Class I indication in the 2011 American guideline. Following the publication of the ISCHAEMIA trial (Maron et al., 2020), Proximal LAD stenosis is no longer considered prognostic and revascularization is only recommended for symptoms. We would anticipate future ESC guidelines would also lead to a downgrade for their recommendations for CABG in the setting of LMS or 3-vessel disease, following the publications of the SYNTAXES and PRECOMBAT 10-year follow-up results.
It is well recognized that the need for repeat revascularization remain higher in those treated with PCI as shown by the PRECOMBAT trial (21.3% with PCI versus 10.6% with CABG at 10 years) (Park et al., 2020). A 2018 review of this topic (Doenst et al., 2019) postulates that this effect is due to “surgical collateralization” in CABG as diseased segments are bypassed entirely. This therefore allows occlusion of these vessels without disruption of myocardial blood flow and therefore with minimal or no clinically relevant sequalae. The fundamental principle of PCI relies upon targeted treatment of flow-limiting stenoses whereas atheromatous coronary lesions may simultaneously have the potential to rupture and cause occlusion without being flow-limiting. In this regard CABG confers a beneficial protective effect over PCI. Further targeted identification and prophylactic treatment of these unstable coronary lesions could be a potential area for future development of PCI. Conversely cerebrovascular event rates are well recognized to be lower in those undergoing PCI when compared to CABG (Head et al., 2018). This is mainly driven by a higher rate (PCI: 0.4%; CABG: 1.1%; HR: 0.33 (95%CI 0.20 – 0.53)) of stroke in the initial 30-day period after CABG and this in turn contributes to higher long-term mortality. Furthermore, CABG is inevitably associated with longer hospital stay and requires the patient to undergo a post-operative recovery period and this may play a role in the decision making for some patients.
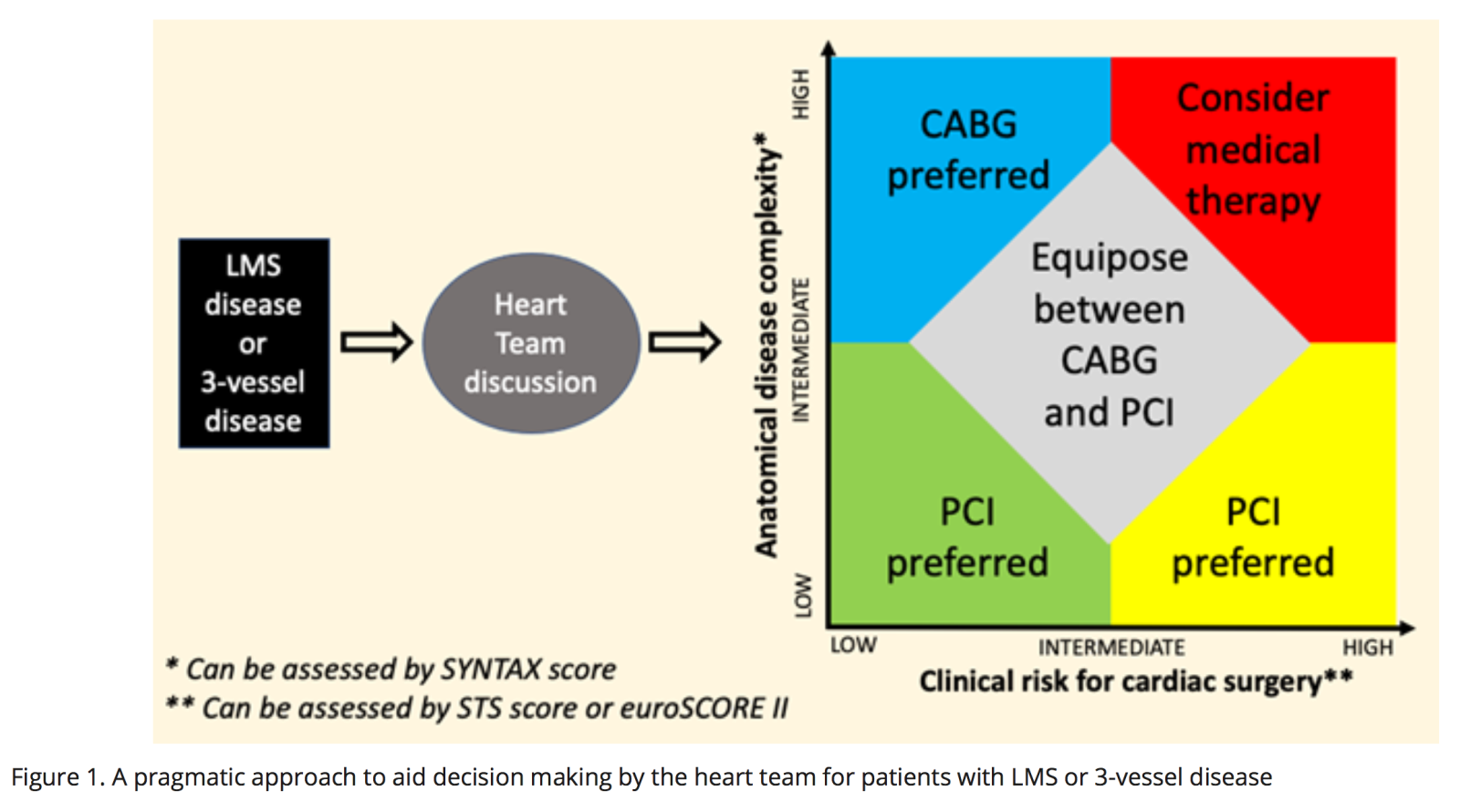
The rapid advancement of PCI technologies makes drawing conclusions from the range of studies complex due to the significant heterogeneity introduced by the variation in stent technology and PCI adjuncts used. In contrast, CABG has changed little in recent times (Melly et al., 2018). One would expect outcomes following PCI would continue to improve, using the latest generation DES with pressure wire-guided and imaged-guided interventions. Ten-year outcomes for the above discussed studies have provided valuable insights. As the primary objective of coronary intervention with either PCI or CABG in those with LMS or multivessel CAD must be to prolong survival, further data with longer term follow-up from studies such as the NOBLE (Nordic-Baltic-British left main revascularization)(Holm et al., 2020) and EXCEL (Xience versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization)(Stone et al., 2019) trials will continue to provide reassurance of our current approach to revascularization by either PCI or CABG for prognostic CAD. A pragmatic approach for now, considering individual disease complexity and the patient’s comorbidities could help the heart team better advise patients on the optimal revascularization strategy as illustrated in Figure 1.
Conclusion
The choice of coronary intervention in modern-day clinical practice is not a one-size-fits-all approach and requires careful consideration of individual patient factors. From the limited evidence published so far, the current data would suggest no mortality benefit at 10 years between PCI and CABG (Woodhead et al., 2022). However, CABG is associated with a 3-fold increased risk of stroke within the first 30 days (Head et al., 2018) and PCI is associated with a 2-fold increased risk of repeat revascularization at 10 years (Park et al., 2020). Diabetic status and coronary disease complexity (SYNTAX score) do not seem to impact on 10-year mortality (Thuijs et al., 2019) but do impact on repeat revascularization. In cases when the heart team considers either PCI or CABG to be equipoise after assessing the anatomical and clinical factors for each patient and depending on local level of expertise to perform complex revascularization, involving the individual patients in the decision-making process may help to offer them the optimal treatment. Longer term outcomes from existing studies are eagerly awaited to strengthen the evidence between PCI and CABG and the interaction between disease location, diabetes status, and CAD complexity.
Competing interests
None of the authors have any competing interests related to this work.
Funding
None
Acknowledgements
None
References
Timothy Woodhead1
1Yorkshire Heart Centre, Leeds General Infirmary, Leeds Teaching Hospitals NHS Trust, Leeds, UK.
Connor Jack Matthews1
1Yorkshire Heart Centre, Leeds General Infirmary, Leeds Teaching Hospitals NHS Trust, Leeds, UK.
Heerajnarain Bulluck*1,2
1Yorkshire Heart Centre, Leeds General Infirmary, Leeds Teaching Hospitals NHS Trust, Leeds, UK. 2Leeds Institute of Cardiovascular and Metabolic Medicine, University of Leeds, Leeds, UK.
Corresponding author:
Heerajnarain Bulluck, PhD
Email: h.bulluck@leeds.ac.uk
In a new window | Download PPT
Figure 1: A pragmatic approach to aid decision making by the heart team for patients with LMS or 3-vessel disease.
Supporting Information
Metrics
| Full-Text | Supporting Information | ||
|---|---|---|---|
| Number | 4643 | 6 | 0 |
Copyright © 2017 Conditioning Medicine, All Rights Reserved.
Address: Conditioning Medicine Editorial Office, 3500 Terrace Street, Pittsburgh, PA, 15213, USA