Browse Articles
Conditioning Medicine
International bi-monthly journal of cell signaling, tissue protection, and translational research.
Current Location:Home / Browse Articles
QT interval duration and dispersion in anorexia nervosa: A systematic review and meta-analysis
Time:2023-12-01
Number:6913
Juhi Rastogi1, Jamie Sin Ying Ho2, Jatin Rastogi3, Jonathan Lazari4, Sarah Davis2, Janice Yiu1, Pooja Jageer1, Niraj S. Kumar1, Ali Kirresh2, Deepa Jain5, Hannah Glatzel6, Grace Kyoko Wong7, Mahmood Ahmad8, Lucaino Candilio2, Florenc Vrapi2, Daniel R. Obaid9, Neil T. Srinivasan10,11, Rui Providência12, Jonathan J. H. Bray9
Author Affiliations


- 1University College London Medical School, London, United Kingdom.
- 2Royal Free London NHS Foundation Trust, London, United Kingdom.
- 3King’s College London Medical School, London, United Kingdom.
- 4Surrey and Sussex Healthcare NHS Trust, Redhill, United Kingdom.
- 5Kent and Medway NHS and Social Care Partnership Trust, Kent, United Kingdom.
- 6Stoke Mandeville Hospital, Aylesbury, United Kingdom.
- 7Department of Materials, University of Oxford, Oxford, United Kingdom.
- 8Tahir Heart Institute, Rabwah, Pakistan.
- 9Institute of Life Sciences, Swansea University Medical School, Swansea, United Kingdom.
- 10Department of Cardiac Electrophysiology, The Essex Cardiothoracic Centre, Basildon, Essex, United Kingdom.
- 11Circulatory Health Research Group, Medical Technology Research Centre, School of Medicine, Anglia Ruskin University, Essex, United Kingdom.
- 12Barts Heart Centre, St Bartholomew’s Hospital, London, United Kingdom
Conditioning Medicine 2023. 6(2): 25-32.
Abstract
Anorexia nervosa (AN) is associated with increased sudden cardiac death with possible prolongation of the QT interval. We aimed to evaluate whether AN is associated with changes in QT interval duration and dispersion. MEDLINE, EMBASE, and COCHRANE databases were systematically searched. The primary endpoint was corrected QT interval (QTc) calculated using the Bazett (QTcB), Hodges (QTcH), Fridericia (QTcF), and Framingham (QTcFr) formulas. The secondary endpoints were QT dispersion (QTd) and QTc dispersion (QTcd). The 28 eligible studies included 2333 patients diagnosed with AN. The meta-analysis of QTcB (mean difference (MD) 5.55 ms, 95% CI -2.38 - 13.48 ms, p = 0.17; 26 studies), QTcH (MD 1.34 ms, 95% CI -8.50 - 11.17 ms, p = 0.79), and QTcF (MD 2.66 ms, 95% CI -13.90 - 19.23 ms, p = 0.75) showed minor prolongation but did not reach statistical significance. The meta-analysis of QTcFr showed a significant QTc prolongation in AN patients (MD 15.90 ms, 95% CI 0.03 - 31.78 ms, p = 0.05, I2 = 65%). Statistically significant higher dispersion values were observed in AN patients vs. controls (QTd: MD 22.30 ms, 95% CI 13.31 - 31.29 ms, p < 0.0001, I2 = 93%; and QTcd: MD 16.93 ms, 95% CI 4.54 - 29.32 ms, p = 0.007 I2 = 93%). AN was not associated with prolongation of QT interval using most correction formulas, but more pronounced QT and QTc dispersion was observed in patients with AN.
Keywords: Anorexia nervosa, QT interval, QT dispersion, Meta-analysis
Abstract
Anorexia nervosa (AN) is associated with increased sudden cardiac death with possible prolongation of the QT interval. We aimed to evaluate whether AN is associated with changes in QT interval duration and dispersion. MEDLINE, EMBASE, and COCHRANE databases were systematically searched. The primary endpoint was corrected QT interval (QTc) calculated using the Bazett (QTcB), Hodges (QTcH), Fridericia (QTcF), and Framingham (QTcFr) formulas. The secondary endpoints were QT dispersion (QTd) and QTc dispersion (QTcd). The 28 eligible studies included 2333 patients diagnosed with AN. The meta-analysis of QTcB (mean difference (MD) 5.55 ms, 95% CI -2.38 - 13.48 ms, p = 0.17; 26 studies), QTcH (MD 1.34 ms, 95% CI -8.50 - 11.17 ms, p = 0.79), and QTcF (MD 2.66 ms, 95% CI -13.90 - 19.23 ms, p = 0.75) showed minor prolongation but did not reach statistical significance. The meta-analysis of QTcFr showed a significant QTc prolongation in AN patients (MD 15.90 ms, 95% CI 0.03 - 31.78 ms, p = 0.05, I2 = 65%). Statistically significant higher dispersion values were observed in AN patients vs. controls (QTd: MD 22.30 ms, 95% CI 13.31 - 31.29 ms, p < 0.0001, I2 = 93%; and QTcd: MD 16.93 ms, 95% CI 4.54 - 29.32 ms, p = 0.007 I2 = 93%). AN was not associated with prolongation of QT interval using most correction formulas, but more pronounced QT and QTc dispersion was observed in patients with AN.
Keywords: Anorexia nervosa, QT interval, QT dispersion, Meta-analysis
Highlights
This study reviews the literature on anorexia nervosa (AN) as it relates to QT interval duration and dispersion in individuals with cardiac failure. Conditioning medicine has been shown to be effective against cardiac failure, suggesting that management of cardiac failure, including AN, may provide insights into the use of conditioning medicine for AN. There is a suspected pathological link between AN, an eating disorder characterized by extreme food restriction and low body weight, and cardiac failure, a condition where the heart is unable to pump blood effectively. Indeed, AN is associated with an increased risk of sudden cardiac death. Prolongation of the QT interval is a cardiac electrophysiological abnormality that can increase the risk of arrhythmias and sudden cardiac death. The literature suggests that AN is not associated with prolongation of the QT interval but more pronounced QT and corrected QT interval dispersion are observed in patients with AN. These observations underscore the importance of monitoring and managing cardiac health in individuals with AN, especially given their higher risk of sudden cardiac death, thereby suggesting utmost consideration when contemplating conditioning medicine for treating this patient population.
Introduction
Anorexia nervosa (AN) has the highest mortality rate among all psychiatric illnesses, with a standardized mortality ratio of 6.2 (Papadopoulos et al., 2009). The mechanisms behind this high rate are poorly understood (Jáuregui-Garrido and Jáuregui-Lobera 2012). Even amongst the estimated third of deaths attributable to cardiac causes, the exact etiology behind their sudden cardiac death remains unclear (Jáuregui-Garrido and Jáuregui-Lobera 2012). Research has focused on if or why AN patients may be predisposed to ventricular arrhythmias. Following the publication of several case reports, one proposed mechanism was via prolongation of the QT interval on electrocardiograms (ECG) (Cooke et al., 1994). In the general population, QT interval prolongation is independently associated with increase in sudden cardiac death, potentially leading to degeneration of stable rhythms into Torsades de Pointes and ventricular fibrillation (Straus et al., 2006). The reasons why AN patients may have a prolonged QT include electrolyte abnormalities, psychotropic medication use, and autonomic dysfunction (Sachs et al., 2016).
However, systematic attempts at demonstrating prolonged QT intervals in individuals with AN remains contradictory. Two meta-analyses exist to date, both focusing on the heart rate (HR) corrected QT interval (QTc) (Lesinskiene et al., 2008; Janzen et al., 2018). Janzen et al. (2018) observed no significant difference in the QTc of patients with AN compared to control subjects, which was contrary to the first meta-analysis by Lesinskiene and colleagues (2008). More recently, there has been focus on QT dispersion (QTd) or QTc dispersion (QTcd), which is defined as the difference between the maximum and the minimum QT/QTc across all ECG leads. However, there has been no pooled analysis of individual trials on QTd/QTcd in the AN population.
Our systematic review therefore has two main aims. First, to help further clarify if AN patients have longer QTc intervals compared to case matched controls by including up to date trials with larger patient numbers. Second, to be the first pooled analysis attempting to ascertain if there may be any increase in QTd/QTcd in the AN population.
Methods
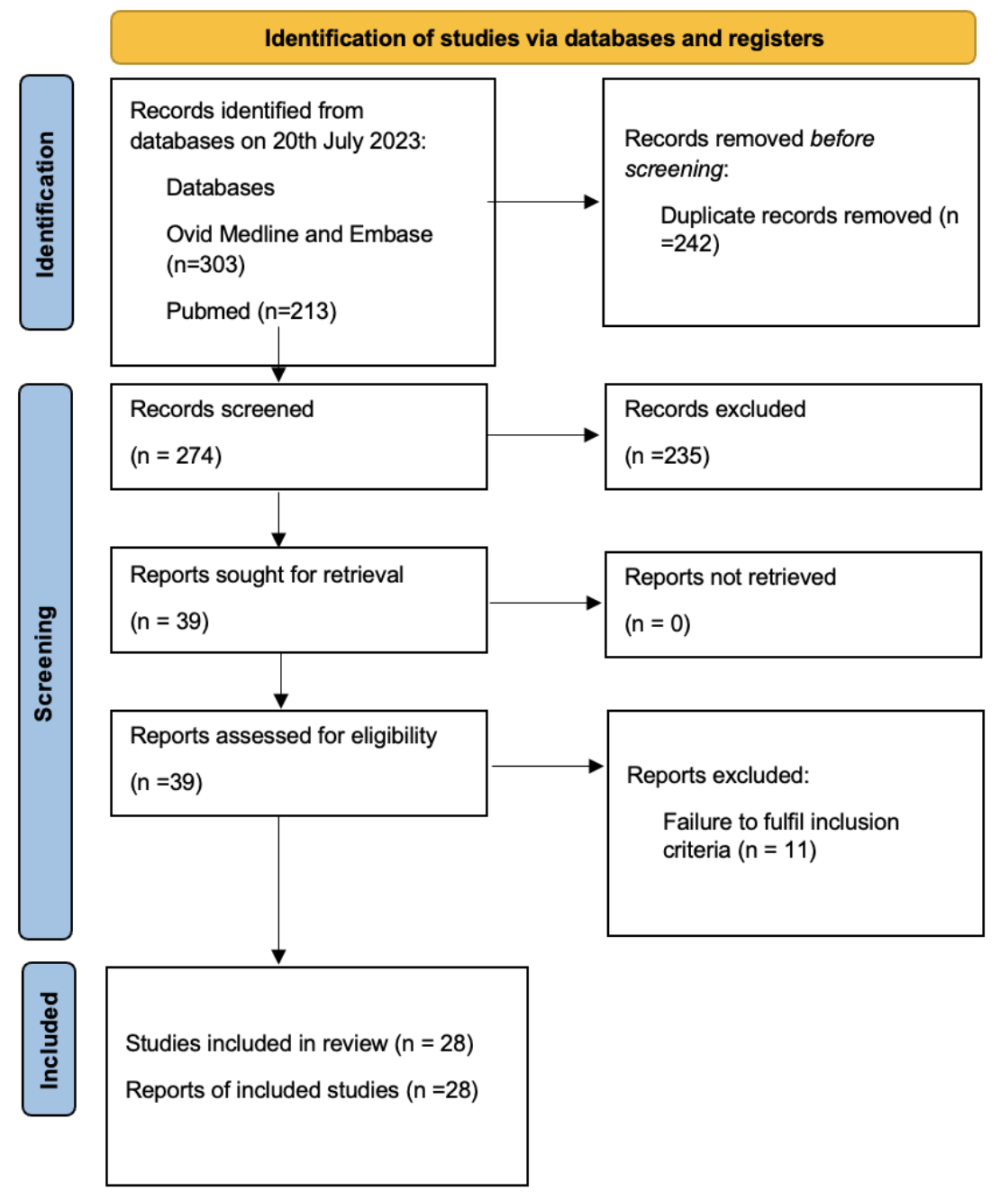
A systematic review of the published literature was performed according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guideline (Page et al., 2021).
Search strategy and selection criteria
MEDLINE, EMBASE, and COCHRANE databases were systematically searched for studies published up to July 20, 2023 using the following search term: (long QT syndrome OR electrocardiography) AND anorexia nervosa. Additional studies were identified from reference searching of included studies. The inclusion criteria were (i) a confirmed diagnosis of AN, and (ii) measurement of QTc interval on 12-lead electrocardiogram (ECG). Studies were excluded if they were conference abstracts not published as full paper within 3 years, non-English language studies, case reports, comments, editorials, systematic reviews, and meta-analyses. In publications from overlapping study populations, the study with the largest cohort was included in the analysis. Three authors (JR, JL, JSR) independently screened records for eligibility based on titles and abstracts, and then performed full-text review for final inclusion. Screening selection discrepancies were resolved via discussion and consensus.
Data extraction and quality assessment
Information was extracted onto pre-defined data forms on total sample size, patient demographics, duration of disease, body mass index (BMI), HR, psychotropic medication use, QTc, QTc formulas used, QTd and/or QTcd values, by two authors independently. Corresponding authors were contacted for clarification and missing data where needed. For each study, two authors independently assessed the quality of non-randomized studies using the Newcastle–Ottawa Scale (NOS). The Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach was used to assess the certainty of the evidence. Discrepancies in data extraction and quality assessment were resolved through discussion and consensus.
Study endpoints
The primary endpoint of the study was QTc calculated using the Bazett (QTcB) formula, which is calculated by QTc = QT (seconds)/√RR (seconds). QTcB is recommended by international guidelines for the diagnosis of long QT syndrome (Priori et al., 2013). It is the most common QTc formula used, therefore it was assumed that the unreported studies used this method (Postema and Wilde 2014). QTc measured using the Hodges (QTcH; QTc = QT (seconds) + 0.00175 × (HR (beats per minute) -60)), Fridericia (QTcF; QTc = QT (seconds)/3√RR (seconds)), and Framingham (QTc = QT (seconds) + 0.154 × (1-RR (seconds))) methods was also assessed as a secondary endpoint in this study as these formulas are known to lead to significant reclassification of presence of long QT compared to QTcB (Vandenberk et al., 2016; Providência et al., 2018). Additional secondary endpoints were QTd and QTcd.
Statistical analysis
Statistical analysis was conducted using Review Manager (RevMan Computer program, Version 5.4.1, The Cochrane Collaboration, 2020). A primary meta-analysis was performed using the DerSimonian-Laird random-effects model to calculate the pooled estimate of the mean differences (MD) in QTc between the AN and control subjects. Forest plots were generated with 95% confidence intervals (95% CIs). The I2 value was used to estimate heterogeneity, with the prespecified cut-offs of low, moderate, and high heterogeneity defined as <25%, 25 - 75%, and >75% respectively. A p-value of <0.05 was considered statistically significant.
Publication bias was assessed using visual inspection of funnel plots for asymmetry and Egger’s regression asymmetry test (Sterne et al., 2011). Subgroup analysis was performed based on the QTc formula used. We also performed subgroup analysis based on categories of AN severity based on BMI (mild: >17 kg/m2; moderate: 16-16.9 kg/m2; severe: 15-15.9 kg/m2; extreme <15 kg/m2), age (above or below mean age), country of origin by continent (Europe, America, or Asia), use of psychotropic medication (above or below mean proportion), HR (above or below median HR), and clinical setting (inpatient, outpatient, or both). A sensitivity analyses based on study quality (cut-off of NOS >7 representing high quality studies) was performed.
Patient and public involvement
The patients nor the public were involved in this research study.
Results
Our systematic search identified 446 articles, from which 28 studies were found to be eligible (Figure 1). All studies were observational, and most studies compared age- and sex-matched controls except for the study by Green et al. (2020) that made comparison to sex-matched controls only. The 28 eligible studies included 2333 AN patients (Table 1). Most of the patients were female (96.3%) with an overall mean age of 19.7 years (95% CI 18.0 to 21.4) and mean duration of disease ranging from 9.1 to 129.6 months. Seven studies reported the proportion of AN participants on psychotropic medications (Nussinovitch et al., 2012; Padfield et al., 2016; Frederiksen et al., 2018; Janzen et al., 2019; 2020; Krantz et al., 2020; Dinardo et al., 2022), four of which included only medications with potential for QTc prolongation (Padfield et al., 2016; Janzen et al., 2020; Krantz et al., 2020; Dinardo et al., 2022) The mean proportion of antipsychotic use was 46.5% (95% CI 14.7 to 78.3) and the pooled mean HR was 60.0 bpm (95% CI 56.9 to 63.0). The method of measurement of QT interval was reported in 22 studies, of which three used computer-assisted calculations (Roche et al., 2004; Roche et al., 2005; Krantz et al., 2020), six used the tangent (or slope intercept) method (Franzoni et al., 2002; Padfield et al., 2016; Bomba et al., 2018; Frederiksen et al., 2018; Janzen et al., 2019, 2020), 12 used the threshold method (Duraković et al., 1994; Nussinovitch et al., 2012; Ulger et al., 2006; Facchini et al., 2006; Olivares et al., 2005; Takimoto et al., 2004; Vázquez et al., 2003; Galetta et al., 2003; Biadi et al., 2001; Panagiotopoulos et al., 2000; Dinardo et al., 2022; Borgia et al., 2021), and one reported performing manual calculation but did not specify the method used (McLaughlin et al., 1995; Krantz et al., 2005).
Quality assessment of the included studies
NOS quality assessment of included studies showed 12 (43%) and 16 (57%) studies deemed to be of fair and high quality, respectively (Supplementary Table 1). GRADE rating of study outcomes indicated low certainty of evidence (Supplementary Table 2) indicating that our confidence in the effect estimates is limited and further research is very likely to change the effect estimate.

AN and QTc interval
The formula used for QTc was reported in 25 studies: Bazett (QTcB) (Duraković et al., 1994; Panagiotopoulos et al., 2000; Biadi et al., 2001; Franzoni et al., 2002; Galetta et al., 2002; Vázquez et al., 2003; Roche et al., 2004; Takimoto et al., 2004; Krantz et al., 2005; Roche et al., 2005; Olivares et al., 2005; Facchini et al., 2006; Ulger et al., 2006; Nussinovitch et al., 2012; Billeci et al., 2015; Padfield et al., 2016; Bomba et al., 2018; Frederiksen et al., 2018; Janzen et al., 2019; Green et al., 2020; Janzen et al., 2020; Krantz et al., 2020; Borgia et al., 2021; Dinardo et al., 2022); Hodges (QTcH; five studies) (Frederiksen et al., 2018; Janzen et al., 2019, 2020); Fridericia (QTcF; four studies) (Frederiksen et al., 2018, 2021; Janzen et al., 2019; Krantz et al., 2020); Framingham (QTcFr; two studies) (Roche et al., 2004; Janzen et al., 2019). Unreported studies (two studies) (Galetta et al., 2003; Yahalom et al., 2013) were assumed to use the Bazett method as it is most commonly used (Postema and Wilde 2014).
The meta-analysis of QTcB values involving 26 studies and 2084 patients showed similar QTcB between AN patients and controls (MD 5.55 ms, 95% CI - 2.38 to 13.48 ms, p = 0.17) (Figure 2A), with very high heterogeneity (I2 = 95%). The mean QTcB of AN and control groups was 403.9 ms (95% CI 397.6 to 410.2 ms) and 398.7 ms (95% CI 390.3 to 407.2 ms), respectively. Analysis of 23 studies that explicitly reported using the Bazett correction showed similar result (MD 4.12 ms, 95% CI -4.34 to 12.58 ms, p = 0.34, I2 = 96%). Similarly, analysis of three studies reporting QTcH on 501 patients showed no significant differences between AN patients and controls (MD 1.34 ms, 95% CI -8.50 to 11.17 ms, p = 0.79) (Figure 2B), with moderate heterogeneity (I2 = 71%). Four studies involving 1368 patients reported QTcF, and there was no significant difference between AN patients and controls (MD 2.66 ms, 95% CI -13.90 to 19.23 ms, p = 0.75) (Figure 2C), with high heterogeneity (I2 = 98%). Two studies involving 63 AN patients reported QTcFr, and the difference between AN patients and controls reached statistical significance (MD 15.90 ms, 95% CI 0.03 to 31.78 ms, p = 0.05) (Figure 2D), with moderate heterogeneity (I2 = 65%).

In a new window | Download PPT
Figure 2. Forest plots of the random effects model of (A) QTcB, (B) QTcH, (C) QTcF and (D) QTcFr. Abbreviations: AN, anorexia nervosa; QTcB, corrected QT interval by Bazett formula; QTcF, corrected QT interval by Fridericia formula; QTcFr, corrected QT interval by Framingham formula; QTcH, corrected QT interval by Hodges formula.
Sensitivity analysis, meta-regression, and subgroup analysis
To explore the factors contributing to the high heterogeneity, a sensitivity analysis including only studies of high quality was performed. This showed no significant difference in QTcB between AN and controls (MD 2.75 ms, 95% CI -5.38 to 10.87 ms; p = 0.51; I2 = 96%).
Meta-regression of the covariates age (regression co-efficient -0.046, 95%; p = 0.965; Supplementary Figure 1), duration of AN (regression co-efficient 0.315; p = 0.426; Supplementary Figure 2), and BMI (regression co-efficient -4.33; p = 0.364; Supplementary Figure 3) showed no significant association with MD in QTcB. Lower HR was significantly associated with increased MD in QTcB (regression co-efficient -1.41; p = 0.025; Supplementary Figure 4).
In a new window | Download PPT
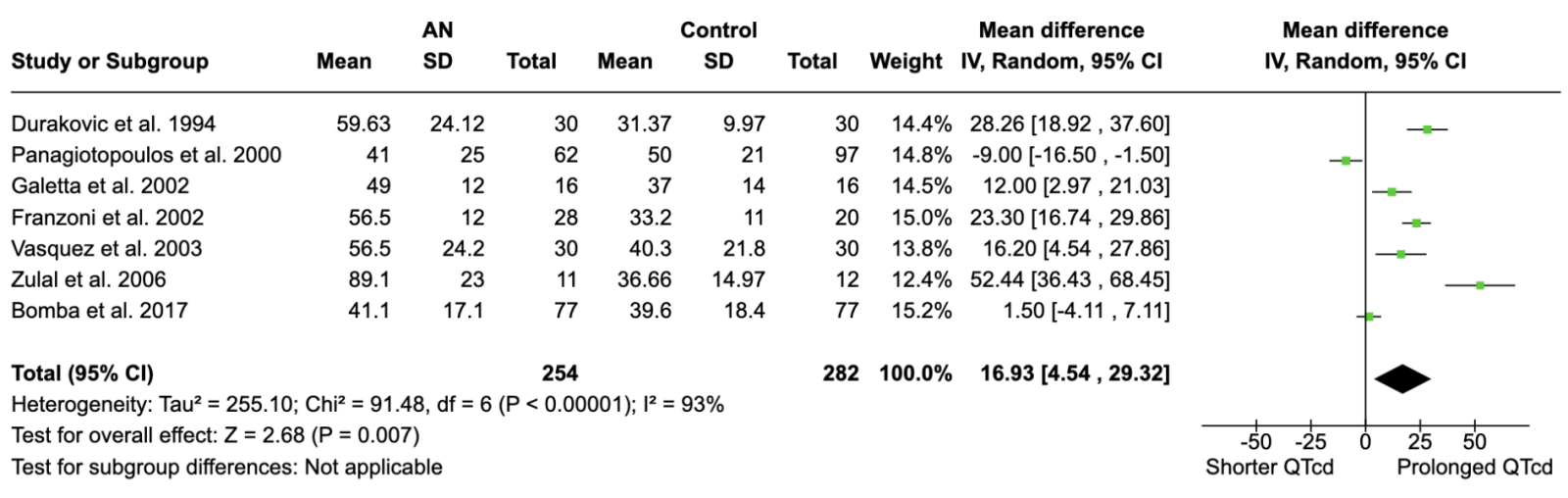
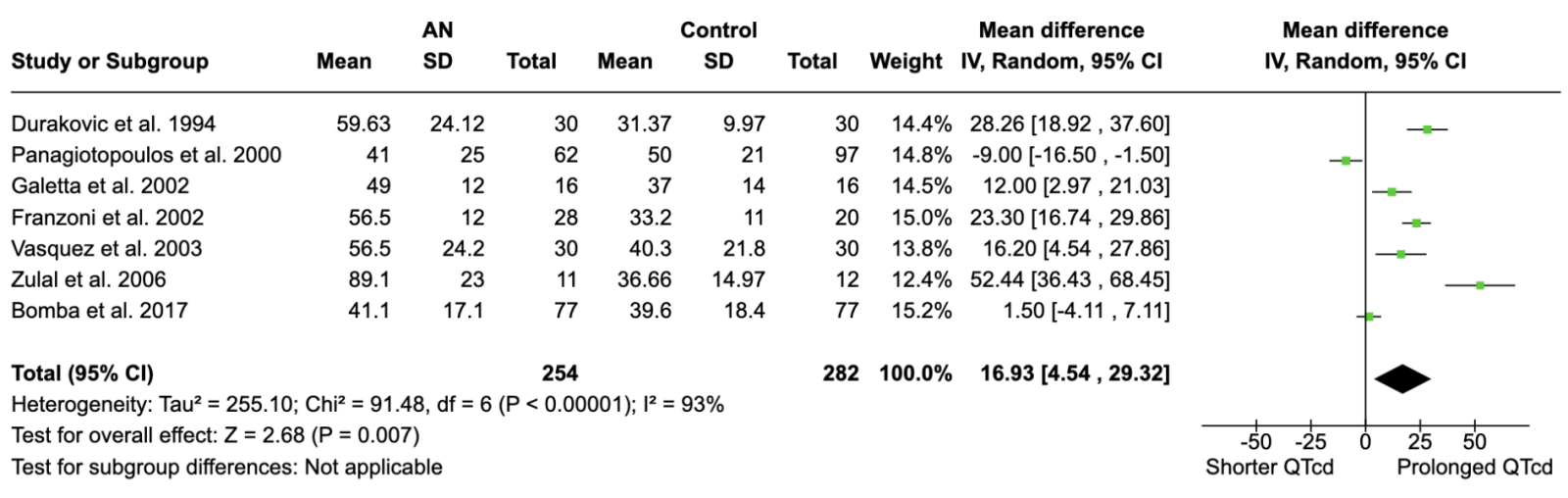
Figure 4. Forest plot comparing QTcd between AN and controls. Abbreviations: AN, anorexia nervosa; QTcd, corrected QT interval dispersion.
Subgroup analysis comparing AN severity based on BMI showed a significant difference between the subgroups (chi2 = 13.10; p = 0.004; I2 = 77.1; Supplementary Figure 5). QTcB was significantly shorter in AN patients with BMI 16 – 17 kg/m2 (MD -10.20 ms, 95% CI -18.38 to -2.02 ms; p = 0.01; I2 = 79%), but significantly longer in patients with BMI 15 – 16 kg/m2 (MD 16.98 ms, 95% CI 4.00 to 29.96 ms; p = 0.01; I2 = 95%). Subgroup analysis comparing patients above or below the pooled mean age of 19.7 years showed no significant differences between the groups (chi2 = 0.06; p = 0.80; I2 = 0%; Supplementary Figure 6). QTcB was significantly longer in AN in studies performed in Asia only (MD 29.44 ms, 95% CI 3.19 to 55.69 ms; p = 0.03; I2 = 93%), but there were significant differences based on continent (chi2 = 6.53; p = 0.04; I2 = 69.4%; Supplementary Figure 7). There was significant difference in QTcB based on antipsychotic use (chi2 = 4.25; p = 0.04; I2 = 76.5; Supplementary Figure 8), mean HR with a cut-off of 60 bpm (chi2 = 1.46; p = 0.23; I2 = 31.6%; Supplementary Figure 9), and clinical setting or acuity of the AN patients (chi2 = 3.74; p = 0.15; I2 = 46.5%; Supplementary Figure 10).
QTd and QTcd associated with AN
QTd values (Figure 3) were reported in nine studies, involving 276 patients. The mean QTd in AN and controls was 56.1 ms (95% CI 47.7 to 64.6 ms) and 33.9 ms (95% CI 26.6 to 41.1ms), respectively. AN patients had significantly higher QTd than controls (MD 21.30 ms, 95% CI 13.31 to 31.29 ms, p < 0.0001; I2 = 93%). QTcd values (Figure 4) were provided in seven studies involving 282 patients. The mean QTcd was 55.3 ms (95% CI 44.1 to 66.6 ms) in the AN group and 38.3 ms (95% CI 33.4 to 43.3 ms) in the control group. QTcd was significantly larger in AN patients than controls (MD 16.93 ms, 95% CI 4.54 to 29.32 ms, p = 0.007; I2 = 93%).

In a new window | Download PPT
Figure 3. Forest plot comparing QTd between AN and controls. Abbreviations: AN, anorexia nervosa; QTd, QT interval dispersion.
In the subgroup analysis based on BMI categories, QTd was significantly increased in AN patients with BMI 15 - 15.9 kg/m2 (MD 24.33, 95% CI 18.19-30.48; p < 0.0001; I2 = 77%) and 16 - 16.9 kg/m2 but not BMI <15 kg/m2 (MD 12.27, 95% CI -3.43-27.97; p = 0.13; I2 = 86%), although only one study had BMI 16 - 16.9 kg/m2 (Supplementary Figure 11). In contrast, for QTcd, only those with BMI 15 - 15.9 kg/m2 (MD 17.85, 95% CI 10.46-25.24; p < 0.0001; I2 = 52%) showed increased QTcd, while QTcd was lower in AN patients with BMI 16 - 16.9 kg/m2 (MD-9, 95% CI -16.50 to -1.50; p = 0.02) (Supplementary Figure 12). However, the number of studies and patients was small in each subgroup, therefore further studies are needed to confirm these findings.
Publication bias
Funnel plot was generated for the meta-analysis of QTcB (Supplementary Figure 13). This plot was asymmetrical with >50% of studies lying outside the triangular region (this encompassed 95% of studies in the absence of bias) (Sterne et al., 2011) There is a suggestion of missing studies in the bottom of the triangle, which would correspond to studies with neutral results, suggesting that reporting bias may have been present for this endpoint.
Discussion
Overall, we found no significant difference between the QTc interval of patients with AN compared with control subjects. This finding remained even when low and medium quality trials were excluded.
There are two prior meta-analyses comparing the QTc of patients with AN to controls (Lesinskiene et al., 2008; Janzen et al., 2018). Our pooled analysis includes more trials (28 vs. 10 and 16) and more patients (2333 vs. 316 and 964). Our findings are consistent with the most contemporaneous and extensive of the prior published meta-analysis, which also did not find a significant prolongation of QTc interval in patients with AN.
QTc and AN: Subgroup analyses
Univariate meta-regression of variables, such as age, duration of illness, and BMI demonstrated no significant association with QTcB and these variables. Interestingly, we did note a significant difference in the QTcB of anorexic patients vs. controls in trials conducted in Asia that requires further analysis and research.
QTc and AN: Limitations
The majority of the included trials have the same limitations as prior meta-analyses. First, there were trial design limitations, with all included trials being retrospective observational studies of small to moderate size. As such, our meta-analysis may be susceptible to confounding factors, selection, and observation bias.
Secondly, there is still a lack of reporting of factors known to alter the QTc such as use of psychotropic medications and electrolyte abnormalities. Some antipsychotic medications are known to prolong the QTc, and over 50% of AN patients are on at least one antipsychotic (Janzen et al., 2018). We attempted to explore this with subgroup analyses, comparing the QTc interval in those trials reporting high rates of antipsychotic use vs. those with low usage. There was no significant difference in the QTc based on the proportion of antipsychotic use. However, we were unable to stratify within these studies whether these patients were on antipsychotics with higher risk of QT prolongation. Additionally, QT prolongation may be dose-dependent and variable gut absorption may also play an important role in creating heterogeneity. However, it is worth noting that most studies in our meta-analysis did not report the proportion of patients on antipsychotics, and only one reported QTc values in the subgroup of AN patients on antipsychotics. As such, this was not something we could analyze but would encourage reporting of in future trials.
Another limitation for discussion is the formula used to correct the QT interval for HR. QT duration is impacted by HR, with slower and faster HR giving longer QT intervals. As such, the QT interval should always be HR corrected (i.e. the QTc) at stable HR. The most commonly used correction formula used is QTcB, which is the recommended formula in the joint European Society of Cardiology, Asia Pacific Heart Rhythm Society, American College of Cardiology, and American Heart Association guidelines for diagnosing long QT syndrome (Priori et al., 2013). However, recent data suggest the QTcB yields significant errors and that QTcF and QTcFr are less prone to error with slow and fast HR (Andršová et al., 2021). This limitation of QTcB is especially relevant in the AN population, in which bradycardia is such a common feature. In addition, QTcB is the least accurate in terms of predicting mortality, with the QTcFr being the most strongly predictive of 30-day and 1-year mortality (Vandenberk et al., 2016). We found that when using QTcFr, there was a significant difference in QTc when comparing AN to case-controls. However, there were only two studies involving 63 patients, and there is a need for more trials in the future using QTcFr. Furthermore, none of the studies reported mortality outcomes, therefore a meta-analysis could not be performed.
QT Dispersion and AN
This is, to the best of our knowledge, the first meta-analysis to ascertain the significance of QTd and QTcd in the AN population. Much like QTc, QTd is associated with life-threatening ventricular arrhythmias, with QTd/QTcd outperforming QTc in its ability to predict in-hospital mortality following out of hospital cardiac arrest (Kosmopoulos et al., 2020). In a trial of 58 anorexic females, QTcd was noted to be longer compared to controls, and prolongation was best predicted by a preceding low weight, low BMI, and rapid weight loss (Swenne and Larsson, 1999). Despite this, QTd itself has never been identified as a marker of sudden cardiac death in larger studies (O’Neal et al., 2017). However, in specific cohorts of patients who are known to be of high risk such as survivors of cardiac arrest, it may be associated with increased risk of sudden cardiac death (Kosmopoulos et al., 2020). Our meta-analysis attempts to build on this. We included nine studies that reported QTd values in 276 patients, and seven studies reporting QTcd values in 282 patients. There was a statistically significant mean difference in the QTd and QTcd between AN patients and controls. Given the prognostic significance that having a prolonged QTd/QTcd appears to carry, and our finding that QTd/QTcd is prolonged in anorexic patients, a more detailed and dedicated investigation is warranted. Specifically, other markers such as T-wave onset to peak, T-peak to T-end and differences of T-wave parameters across ECG leads may allow for more specificity in looking for subtle markers of repolarization heterogeneity and differences in this cohort (O’Neal et al., 2017) These markers are not routinely included in standard ECG assessments and are hard to replicate without computational software, resulting in limited inclusion in studies.
Other causes of sudden cardiac death
It’s important to take the results of this meta-analysis in the clinical context. Although QTc prolongation has biological plausibility in AN, our meta-analysis found no significant QTc prolongation in the AN population as a whole. Therefore, perhaps the focus needs to shift outside of the QTc interval. QT dispersion seems a logical next step given our above results and we hope future trials report specifically on QTd/QTcd. Most of the ECG assessments were conducted in static situations, however, QT prolongation can be dynamic, often exacerbated by exercise and stress, or extreme bradycardia. The lack of studies assessing abnormal QT prolongation dynamically may explain why the current data fail to demonstrate an association between QT prolongation and sudden cardiac death in AN.
Although outside the scope of this meta-analysis, there are numerous other plausible pathophysiological mechanisms for ventricular arrhythmias in patients with AN. For example, they have reduced left ventricular mass with reduced chamber dimensions, high rates of mitral valve prolapse, and increased late gadolinium enhancement on cardiac magnetic resonance imaging (Sachs et al., 2016) This should not detract from viewing the anorexic patient with a prolonged QTc very seriously, with rigorous searching for potential secondary drivers, and consideration of admission for cardiac monitoring.
Conclusion
First, our meta-analysis demonstrated no significant difference in the QTc of patients with AN compared to control. Second, our results, however, do suggest that individuals with AN may be more likely to have prolonged QTc if corrected using the Framingham formula relative to controls. Third, the QTd and QTcd were significantly increased in patients with AN compared with controls. Lastly, there is still a lack of reporting of factors known to alter the QTc interval such as the use and dose of psychotropic medications and electrolyte abnormalities. We suggest further trials report using multiple QTc formulas, or publish raw QT intervals and HR data, to allow for comparisons.
Conflict of interest
None declared.
References
Juhi Rastogi1
1University College London Medical School, London, United Kingdom.
Jamie Sin Ying Ho2
2Royal Free London NHS Foundation Trust, London, United Kingdom.
Jatin Rastogi3
3King’s College London Medical School, London, United Kingdom.
Jonathan Lazari4
4Surrey and Sussex Healthcare NHS Trust, Redhill, United Kingdom.
Sarah Davis2
2Royal Free London NHS Foundation Trust, London, United Kingdom.
Janice Yiu1
1University College London Medical School, London, United Kingdom.
Pooja Jageer1
1University College London Medical School, London, United Kingdom.
Niraj S. Kumar1
1University College London Medical School, London, United Kingdom.
Ali Kirresh2
2Royal Free London NHS Foundation Trust, London, United Kingdom.
Deepa Jain5
5Kent and Medway NHS and Social Care Partnership Trust, Kent, United Kingdom.
Hannah Glatzel6
6Stoke Mandeville Hospital, Aylesbury, United Kingdom.
Grace Kyoko Wong7
7Department of Materials, University of Oxford, Oxford, United Kingdom.
Mahmood Ahmad8
8Tahir Heart Institute, Rabwah, Pakistan.
Lucaino Candilio2
2Royal Free London NHS Foundation Trust, London, United Kingdom.
Florenc Vrapi2
2Royal Free London NHS Foundation Trust, London, United Kingdom.
Daniel R. Obaid9
9Institute of Life Sciences, Swansea University Medical School, Swansea, United Kingdom.
Neil T. Srinivasan10,11
10Department of Cardiac Electrophysiology, The Essex Cardiothoracic Centre, Basildon, Essex, United Kingdom. 11Circulatory Health Research Group, Medical Technology Research Centre, School of Medicine, Anglia Ruskin University, Essex, United Kingdom.
Rui Providência12
12Barts Heart Centre, St Bartholomew’s Hospital, London, United Kingdom.
Jonathan J. H. Bray9
9Institute of Life Sciences, Swansea University Medical School, Swansea, United Kingdom.
Corresponding author:
Dr. Jamie Sin Ying Ho
Email: sinyingh@gmail.com

In a new window | Download PPT
Figure 2. Forest plots of the random effects model of (A) QTcB, (B) QTcH, (C) QTcF and (D) QTcFr. Abbreviations: AN, anorexia nervosa; QTcB, corrected QT interval by Bazett formula; QTcF, corrected QT interval by Fridericia formula; QTcFr, corrected QT interval by Framingham formula; QTcH, corrected QT interval by Hodges formula.

In a new window | Download PPT
Figure 3. Forest plot comparing QTd between AN and controls. Abbreviations: AN, anorexia nervosa; QTd, QT interval dispersion.
In a new window | Download PPT
Figure 4. Forest plot comparing QTcd between AN and controls. Abbreviations: AN, anorexia nervosa; QTcd, corrected QT interval dispersion.
Metrics
| Full-Text | Supporting Information | ||
|---|---|---|---|
| Number | 6913 | 14 | 5 |
Copyright © 2017 Conditioning Medicine, All Rights Reserved.
Address: Conditioning Medicine Editorial Office, 3500 Terrace Street, Pittsburgh, PA, 15213, USA