Browse Articles
Conditioning Medicine
International bi-monthly journal of cell signaling, tissue protection, and translational research.
Current Location:Home / Browse Articles
Nanoparticle delivery of cardioprotective therapies
Time:2020-02-29
Number:12551
Abraham Mendez-Fernandez1,2, Hector A. Cabrera-Fuentes1,2,3,4,5,6, Bhaarathy Velmurugan2,4, Jason Irei7, William A. Boisvert7, Shengjie Lu2,3, Derek J. Hausenloy2,4,8,9,10
Author Affiliations


- 1Tecnologico de Monterrey, Centro de Biotecnologia-FEMSA, Nuevo Leon, Mexico.
- 2National Heart Research Institute Singapore, National Heart Centre, Singapore.
- 3SingHealth Duke-NUS Cardiovascular Sciences Academic Clinical Programme, Duke-National University of Singapore Medical School, Singapore.
- 4Cardiovascular and Metabolic Disorders Program, Duke-National University of Singapore Medical School, Singapore.
- 5Institute of Fundamental Medicine and Biology, Kazan (Volga Region) Federal University, Russian Federation.
- 6Institute of Physiology, Medical School, Justus-Liebig-University, Germany.
- 7Center for Cardiovascular Research, John A. Burns School of Medicine, University of Hawaii, USA.
- 8The Hatter Cardiovascular Institute, Institute of Cardiovascular Science, University College London, UK.
- 9Yong Loo Lin School of Medicine, National University Singapore, Singapore.
- 10Cardiovascular Research Center, College of Medical and Health Sciences, Asia University, Taiwan.
Conditioning Medicine 2020. 3(1):18-30.
Abstract
Acute myocardial infarction (AMI), and the heart failure (HF) that often follows, are leading causes of death and disability worldwide. Crucially, there are currently no effective treatments, other than myocardial reperfusion, for reducing myocardial infarct (MI) size and preventing HF following AMI. Thus, there is an unmet need to discover novel cardioprotective therapies to reduce MI size, and prevent HF in AMI patients. Although a large number of therapies have been shown to reduce MI size in experimental studies, the majority have failed to benefit AMI patients. Failure to deliver cardioprotective therapy to the ischemic heart in sufficient concentrations following AMI is a major factor for the lack of success observed in previous clinical cardioprotection studies. Therefore, new strategies are needed to improve the delivery of cardioprotective therapies to the ischemic heart following AMI. In this regard, nanoparticles have emerged as drug delivery systems for improving the bioavailability, delivery, and release of cardioprotective therapies, and should result in improved efficacy in terms of reducing MI size and preventing HF. In this article, we provide a review of currently available nanoparticles, some of which have been FDA-approved, in terms of their use as drug delivery systems in cardiovascular disease and cardioprotection.
Abstract
Acute myocardial infarction (AMI), and the heart failure (HF) that often follows, are leading causes of death and disability worldwide. Crucially, there are currently no effective treatments, other than myocardial reperfusion, for reducing myocardial infarct (MI) size and preventing HF following AMI. Thus, there is an unmet need to discover novel cardioprotective therapies to reduce MI size, and prevent HF in AMI patients. Although a large number of therapies have been shown to reduce MI size in experimental studies, the majority have failed to benefit AMI patients. Failure to deliver cardioprotective therapy to the ischemic heart in sufficient concentrations following AMI is a major factor for the lack of success observed in previous clinical cardioprotection studies. Therefore, new strategies are needed to improve the delivery of cardioprotective therapies to the ischemic heart following AMI. In this regard, nanoparticles have emerged as drug delivery systems for improving the bioavailability, delivery, and release of cardioprotective therapies, and should result in improved efficacy in terms of reducing MI size and preventing HF. In this article, we provide a review of currently available nanoparticles, some of which have been FDA-approved, in terms of their use as drug delivery systems in cardiovascular disease and cardioprotection.
1. Introduction
Cardiovascular disease (CVD) is the leading cause of death and disability worldwide, with a major manifestation being acute myocardial infarction (AMI) (Thygesen et al., 2018), a major complication of which is adverse left ventricular (LV) remodelling, and heart failure (HF). Although improvements in AMI treatment have seen a decline in mortality, an increasing number of patients still go on to develop heart failure (Benjamin et al., 2018, 2019). HF impacts significantly on patient morbidity and quality of life, exerting a huge healthcare and economic burden on society. The size of the myocardial infarct (MI), adverse LV remodelling, and the extent of LV dysfunction are the strongest predictors of mortality following AMI. There remains a clinical unmet need, therefore, to discover novel therapies for reducing MI size and preventing adverse LV remodeling, so as to reduce the risk of developing HF and improve survival in AMI patients. Although, a large number of therapies, which have been shown to be effective in the pre-clinical setting in animal AMI models have failed to improve clinical outcomes in the clinical setting in AMI patients (Cung et al., 2015; Bonora et al., 2019; Kleinbongard et al., 2019).
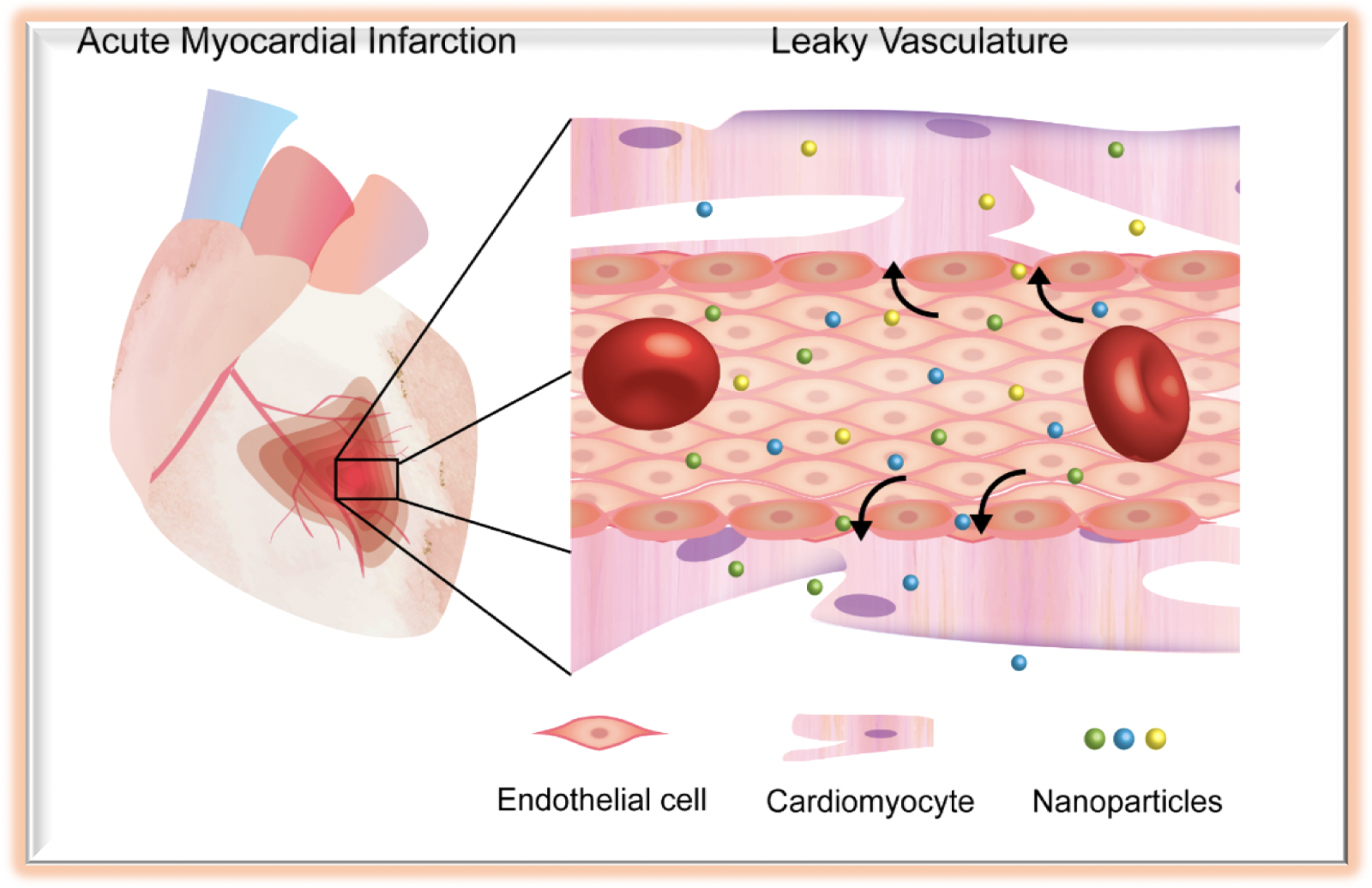
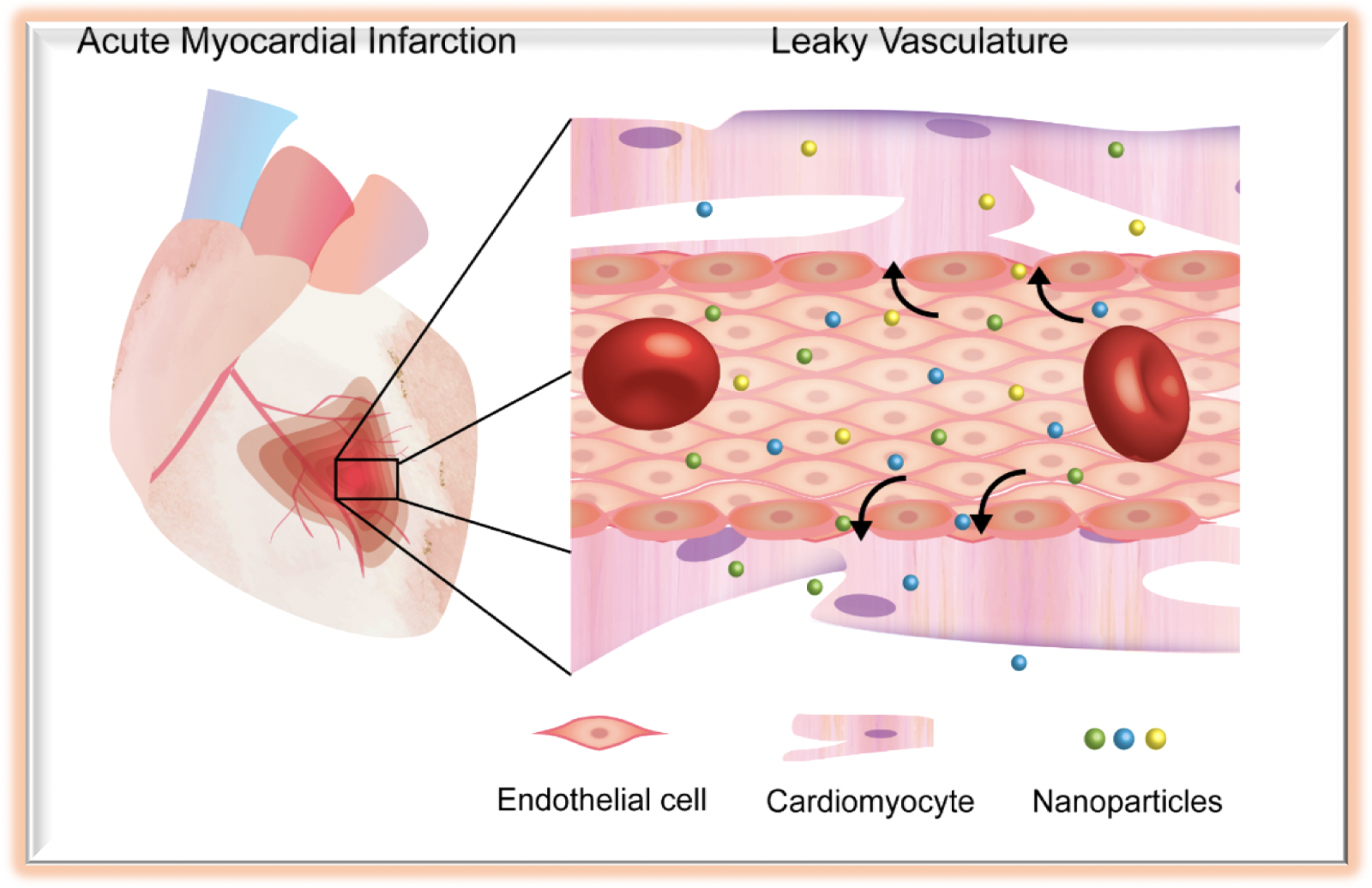
One major reason for this failure to translate cardioprotection into the clinical setting for patient benefit, is the failure to deliver the cardioprotective drug into the ischemic myocardium at sufficient concentrations to be efficacious. In this regard, development of nanoparticles (NPs) as drug delivery systems (DDSs) (Rudramurthy and Swamy, 2018), have the potential to increase the bioavailability and delivery of cardioprotective therapies to the ischemic heart in the setting of AMI, thereby increasing cardioprotective efficacy, and reducing the risk of off-target side effects (Figure 1) (Bhatia, 2016). At present, there are some Food and Drug Administration (FDA)-approved nanomedicines, mostly based on liposomal, polymeric, and nanocrystal formulations. However, trends are changing and nanoparticles composed of other materials have been undergoing clinical trials in recent years (Bobo et al., 2016). The present article provides an update on recent advances in nanoparticle research as drug carriers for therapies, which have the potential to reduce MI size, prevent adverse LV remodeling, and reduce the risk of HF in AMI patients.
In a new window | Download PPT
Figure 1: Schematic illustration of nanoparticle delivery in acute myocardial infarction.
2. Nanoparticles and cardioprotection
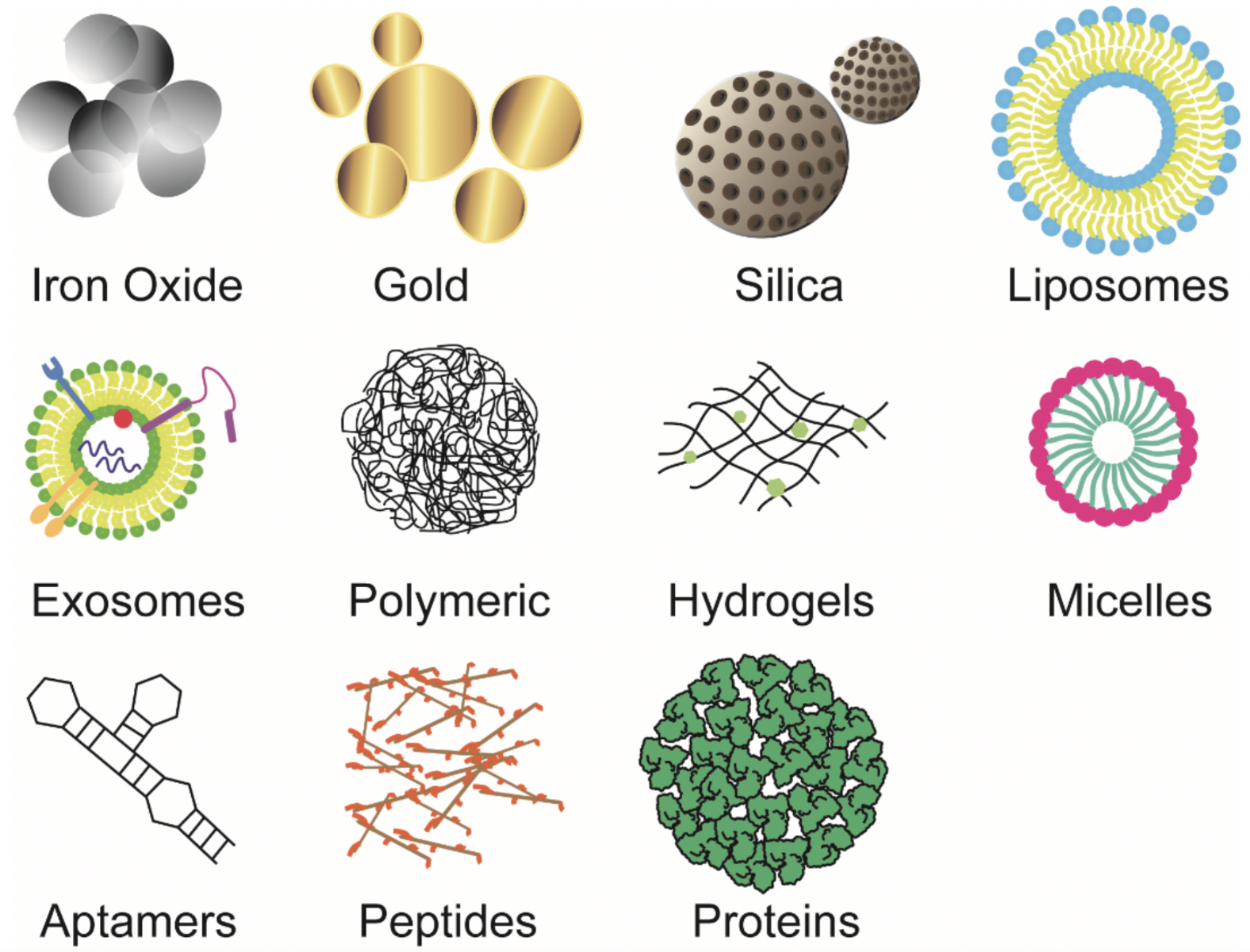
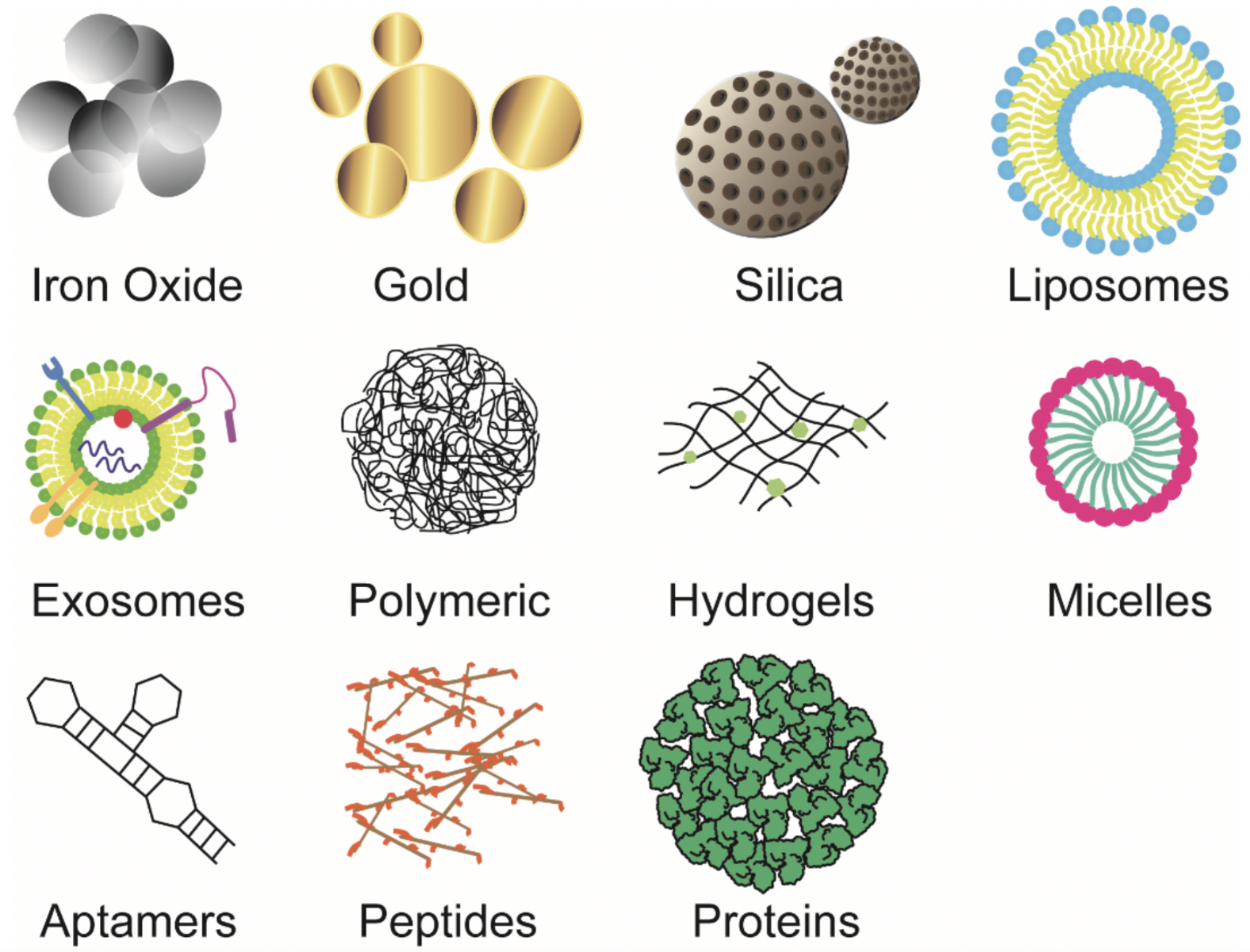
Nanoparticles can be categorized into organic and inorganic subtypes, among which many have been applied to the treatment of CVD including AMI. These include iron oxide NPs, gold NPs (AuNPs), silica NPs, liposomes (exosomes), polymeric NPs, micelles, hybrid hydrogel NPs, and biomolecule-based NPs (Figure 2). The advantages and disadvantages of these different NPs as DDSs are summarized in Table 1.
In a new window | Download PPT
Figure 2: Schematic structure of various nanoparticles that have been applied as drug delivery systems in cardiovascular disease and cardioprotection.
Table 1. The advantages and disadvantages of different types of nanoparticles as a drug delivery system (DDS).
2.1. Inorganic nanoparticles
Magnetic iron oxide nanoparticles
Cardiovascular magnetic resonance (CMR) is the imaging modality of choice for quantifying LV function and MI size, and for assessing the efficacy of novel cardioprotective therapies in AMI patients (Ibanez et al., 2019). NPs offer several possibilities for CMR as contrast agents (Grimaldi et al., 2019), with paramagnetic iron oxide NPs (IONs) leading this technology field. Animal studies have shown that modifications of IONs make it possible to selectively track processes that accompany an AMI, such as cell death, inflammation, angiogenesis, and LV remodeling. Cross-linked IONs coupled to annexin have been used to detect apoptosis in the heart following AMI (Sosnovik et al., 2005). When used in conjunction with a gadolinium chelate, it was possible to differentiate in vivo between necrotic and apoptotic myocardium (Sosnovik et al., 2009). Subsequent studies have shown smaller IONs containing annexin A5 with faster pharmacokinetics, thereby reducing the time between administration and actual imaging (Figge et al., 2014). Iron oxide microparticles tagged with a VCAM antibody have been used to visualize myocardial vasculature in the rat heart following AMI, with areas devoid of signal depicting areas of activated vasculature in the infarcted area (Grieve et al., 2013). As promising as targeted IONs may seem, they have some limitations as they remain in nonliving cells for longer time than expected. Besides, it is impossible to distinguish between IONs and endogenous iron signals coming from intramyocardial hemorrhage (Sosnovik and Caravan, 2019).
A few studies in humans have been conducted to evaluate IONs as CMR contrast agents. An early trial to test ferucarbotran, which is based on superparamagnetic IONs, concluded that no benefits were achieved over gadolinium-based contrast agents in terms of imaging infarction in both ST-segment elevation myocardial infarction (STEMI) and non- ST-segment elevation myocardial infarction patients (Yilmaz et al., 2013b). This could have been due to the dose of iron applied (Yilmaz et al., 2013a). Later, as a proof of concept, ferumoxytol, a formulation of ultra-small superparamagnetic IONs coated with carboxymethyl-dextran was administered intravenously to ten STEMI patients. Ferumoxytol improved the contrast at the infarcted area with no reported adverse effects, although it tended to accumulate in remote myocardium as well as in liver and spleen (Alam et al., 2012). Ferumoxytol was also tested in a clinical trial of fourteen STEMI patients and yielded good results in terms of safety and visualization of the infarcted myocardium (Yilmaz et al., 2013a). Currently, Feraheme (ferumoxytol) is approved by the FDA, but only indicated as an iron deficiency treatment.
Gold nanoparticles
Gold nanoparticles (AuNPs) have demonstrated moderate potential to confer protection in the isoproterenol-induced cardiac injury rat model (Vinodhini et al., 2014; Ahmed et al., 2017). However, there have been reports of cardiotoxicity with strong dependence on the size of the particles and the duration of exposure, when administered via intraperitoneal injection (Abdelhalim, 2011). It has been reported that 40 nm AuNPs can produce significant changes in the normal process of ventricular repolarization, whereas 5 nm particles might affect depolarization. AuNPs (100 nm) were shown to produce left ventricle hypertrophy, and AuNPs were demonstrated to decrease cardiac output and cause apoptosis and fibrosis, irrespective of size (Zhang et al., 2018). Conjugation of AuNPs with polyethylene glycol (PEG) may reduce toxicity, with PEGylated AuNPs shown to not affect LV function and structure after seven days of daily administration (Yang et al., 2013). Under chronic exposure, 10 nm PEGylated AuNPs administration for 2 weeks did increase LV mass but this reverted to basal values after four and twelve weeks of chronic administration (Yang, Tian, & Li, 2016). Remarkably, PEGylated AuNPs tend to accumulate in the fibrotic heart but not in the healthy heart (Yang et al., 2019). Consistent with this finding, the amount of PEGylated gold nano-rods located in the heart of transgenic mice that expressed TNF-α under the α-myosin heavy chain promoter were three times larger than in wild type animals (Higuchi et al., 2019). As a DDS, AuNPs have been shown to prevent progression to doxorubicin-induced heart failure, whether or not conjugated to levosimendan. Intriguingly, it was demonstrated that ultrasound intensified cardiomyocyte uptake of AuNPs, with selective accumulation in the mitochondria (Spivak et al., 2013). Under a regime of short-term dosing of isoproterenol, PEGylated AuNPs downregulated the β1 adrenergic receptor and IL-6 in myocardium and hence, lessened the hypertrophic effects of isoproterenol (Qiao et al., 2017). As a novel strategy, AuNPs loaded with a DNAzyme that specifically cleaves TNF-α mRNA had a pronounced local anti-inflammatory effect. Such an effect correlated with an amelioration in LV function in a rat model of permanent ligation of the left descending coronary artery (Somasuntharam et al., 2016).
Silica nanoparticles
Silica NPs are regarded as attractive DDS because their porous texture permits the loading of significant amounts of drugs (Mehmood et al., 2017). These NPs have been used to deliver cardioprotective therapies to the ischemic heart following AMI. Adenosine adsorbed at the surface of silica NPs have been shown to accumulate passively in the ischemic-region of the heart in a rat model, and confer postconditioning-like protection against acute ischemia/reperfusion injury (IRI) (Galagudza et al., 2012). In another case, curcumin attached to mesoporous silica NPs elevated the serum levels of antioxidant enzymes and conferred protection to myofibril organization in rats with doxorubicin-induced cardiomyopathy (Yadav et al., 2019). Strikingly, in a zebrafish heart failure model, mesoporous silica NPs coupled with a hydrogen peroxide probe allowed the controlled release of captopril under hydrogen peroxide stimulation and improved cardiac function (Tan et al., 2017). A similar approach had been used to control the release of curcumin by means of light or heat-sensitive silica NPs (Yan et al., 2012). As with NPs of other compositions, further functionalization might enable porous silicon NPs to selectively attain heart cells (Ferreira et al., 2016; Ornelas-Soto et al., 2017).
In the area of stem cell therapy, it has been shown that stem cell distribution to the heart following intramyocardial engraftment can be assessed by tracking fluorescently labeled silica NPs. Notably, engulfment of silica NPs by human mesenchymal stem cells does not appear to alter the stemness potential nor the proliferative capacity of the stem cells (Gallina et al., 2015).
However, silica NPs have been reported to be cardiotoxic. When administered to rats via intratracheal applications, silica NPs produced dose-dependent alterations in the myocardium, mainly in mitochondrial structure, which became swollen and had disintegrated cristae (Du et al., 2019). Additionally, in the same preparation, silica NPs increased the serum concentration of pro-inflammatory cytokines and oxidative stress biomarkers as well as heart silicon content (Du et al., 2013). These findings are consistent with in vitro observations in H9c2 cells, where silica NPs induced loss in viability, presumably due to oxidative stress (Ye et al., 2010). In contrast, other studies did not show toxic effects with silica NPs and organomodified silica NPs, although toxicity was only assessed acutely, by measuring heart rate and hemodynamic parameters (Galagudza et al., 2010; Sonin et al., 2015).
2.2. Organic or Natural nanoparticles
Liposomes and exosomes
Liposomes are phospholipidic spherical structures consisting of one or multiple bilayers that, because of their physico-chemical properties, can be loaded with either hydrophilic or hydrophobic materials (Alavi et al., 2017). Liposomes are perhaps the most studied nanocarriers. Numerous animal studies have shown that liposomes are able to deliver to the myocardium a plethora of molecules that preserve cardiac function after an ischemic event, such as adenosine (Takahama et al., 2009), erythropoietin/granulocyte-colony stimulating factor (Yamada et al., 2019), miRNAs (Higashi et al., 2015), oligonucleotides (Liu et al., 2014), and even plant derivatives (Allijn et al., 2017).
One of the crucial advantages of liposomes is that they can be easily tailored for controlled biological interactions, rendering them highly versatile vehicles (Hu et al., 2015). For instance, it has been shown that adding antibodies against cardiac troponin I to liposomes conferred specificity to damaged myocardium (Liu et al., 2014). In this same line, ligands of the angiotensin II type I receptor attached to liposomes provided specificity towards the infarcted heart (Dvir et al., 2011). Interestingly, by using in vivo phage display screening, (Dasa et al. 2015) identified a considerable amount of seven-residue peptides that could direct liposomes to various cell types (cardiomyocytes, endothelial cells, myofibroblasts) at the infarct zone and borderline area. Furthermore, liposomes are susceptible to more than one modification. Wang et al. (2017) appended both a peptide that ensured specific delivery and the HIV-derived cell penetrating peptide TAT to the surface of a liposome. This design gave better results than either modification alone in terms of cardiomyocyte uptake.
Circulating leukocytes are another potential target for attenuating cardiac damage following acute IRI. In this respect, liposomes with encapsulated siRNA against the CCR2 receptor significantly reduced inflammatory monocyte infiltration in mice myocardium subjected to AMI. As expected, this correlated with reduced MI size (Leuschner et al., 2011; Dutta and Nahrendorf, 2015). Furthermore, despite claims regarding the poor efficiency of liposomes as siRNA carriers (Sahay et al., 2013), significant improvements in the field have been achieved through the synthesis of novel lipidic compounds. Uemura et al. (2019) synthesized lipid NPs composed of an original cationic lipid. Anti-CD45 siRNA entrapped in these NPs was effectively delivered to phagocytic cells. Knockdown efficiencies were as high as 91% in cultured macrophages and 30% in mice circulating phagocytes. Of note, in the clinical setting, liposomal prostaglandin E1 administered intravenously immediately after percutaneous coronary intervention (PCI) protected coronary microcirculation and reduced major adverse cardiac events within six months of follow-up in STEMI patients (Wei et al., 2015). Likewise, in unstable angina patients that underwent PCI, that same formulation lowered periprocedural myocardial injury within 24 hours after PCI (Fan et al., 2015).
Similar to liposomes in structure, exosomes are naturally occurring extracellular vesicles in nano-size implicated in intercellular communication (Pegtel and Gould, 2019). Exosomes have been demonstrated to play a cardioprotective role in ischemic heart disease and represent potential therapeutic agents (Yellon and Davidson, 2014; Davidson et al., 2017). Indeed, mesenchymal stem cell derived exosomes appear to act via the same pathways as ischemic conditioning, namely through the activation of the reperfusion injury salvage kinase (RISK) pathway (Arslan et al., 2013). Furthermore, remote ischemic preconditioning has been shown to modestly raise the levels of circulating extracellular vesicles in human patients (Frey et al., 2019). Among the many mediators to be found in exosomes, miRNAs have enticed much interest. Exosomes containing miR-21 and miR-146a are thought to be the responsible entities that promote angiogenesis, cardiomyocyte survival, and cardiac regeneration following cardiosphere derived cell transplantation (Ibrahim et al., 2014; Xiao et al., 2016; Gallet et al., 2017). Moreover, various stimuli (oxidative stress, hypoxia, shockwave therapy) have proven to be effective in triggering the release of miRNA-enriched exosomes, both in vitro and in vivo, with beneficial effects on cardiac function (Xiao et al., 2016; Zhu et al., 2018; Gollman-Tepeköylü et al., 2019). These findings suggest the possibility of therapeutically inducing regeneration, circumventing the need for actual cell transplantation. Nevertheless, one limitation of these studies is that delivery of exosomes depends on direct intramyocardial injection. To overcome poor retention, Vandergrieff et al. (2018) tagged exosomes with a cardiac homing peptide, which led to specific accumulation at the heart after intravenous application. If exosomes are to be translated into the clinical setting, a better understanding of their physiological role, pharmacokinetics, pharmacodynamics, and a more reliable way of isolating them from other extracellular vesicles must be sought (Davidson et al., 2017).
Polymeric nanoparticles
Polymeric NPs encompass a large list of natural and synthetic polymeric materials capable of transporting drugs either encapsulated or adsorbed on their surface (El-Say and El-Sawy, 2017). Amid the vast amount of materials, the copolymer Poly (lactic-co-glycolic acid) (PLGA) has several advantages. PLGA exhibits biocompatibility, biodegradability, and offers the chance of sustained release and targeted delivery. Importantly, PLGA usage is currently approved by the FDA and the European Medicines Evaluation Agency (EMEA) (Danhier et al., 2012; Sharma et al., 2016). Here we provide some relevant examples of PLGA NPs as a bioabsorbable DDS in CVD.
PLGA NPs are able to ferry vascular endothelial growth factor (VEGF) to the infarcted heart and once there, release the growth factor in a sustained manner. Regardless of the size, nano and micrometer-sized PLGA particles (115 nm vs. 4.89 μm) have been shown to significantly increase vascular density in acute myocardial IRI rodent models (Simoń-Yarza et al., 2013; Oduk et al., 2018). Moreover, when VEGF-PLGA microparticles were given in combination with orally administered coenzyme Q10-PLGA NPs, a further improvement in the ejection fraction was achieved (Simoń-Yarza et al., 2013). Insulin-like growth factor (IGF) incorporated into PLGA NPs distributed mainly at the heart and gave better results when compared to freely infused IGF in terms of cardioprotection (Chang et al., 2013). Other growth factors such as neuregulin and fibroblast growth factor 1 (FGF1) had similar favorable effects on vessel formation and maturation, and enhanced systolic function when embedded in PLGA formulations (Pascual-Gil et al., 2017). PLGA microparticles loaded with antagomir-92a have been used to downregulate the anti-angiogenic miR92a in a swine myocardial IRI model, and resulted in enhanced angiogenesis and less adverse LV remodeling (Bellera et al., 2014). Apart from directly increasing vessel density and cardiomyocyte survival, another feasible cardioprotective strategy is attenuating inflammation. PLGA-pioglitazone has been shown to reduce adverse post-AMI LV remodeling by decreasing the proportion of M1/M2 macrophages in the post-infarcted mouse and pig hearts (Tokutome et al., 2019). In a similar manner, pitavastatin bound to PLGA particles, but not pitavastatin in solution, prevented post-AMI adverse LV remodeling by inhibiting inflammatory monocyte recruitment (Mao et al., 2017). Targeting the opening of the mitochondrial permeability transition pore (MPTP), a critical determinant of cardiomyocyte death following acute IRI, PLGA particles conjugated to cyclosporine A resulted in a greater reduction in MI size when compared to cyclosporine A alone (Ikeda et al., 2016). Furthermore, the addition of the Szeto-Schiller 31 peptide to cyclosporine A increased the accumulation of cyclosporine A at the inner mitochondrial membrane, and increased cardioprotective efficacy (Zhang et al., 2019).
In addition to PLGA-based polymeric NPs, cyclodextrin-based NPs are also suitable systems for drug delivery. Cyclodextrins are carbohydrates composed of several units of glucose. Ingestion of cyclodextrins is considered safe by the FDA. Nonetheless, parenteral administration is restricted to a few cases because of hemolysis, as well as hepatic and renal toxicity (Braga, 2019). Cyclodextrin-based nanosponges are hyper-crosslinked polymeric particles that resemble porous spheres made of interlinked cyclodextrins. Nanosponges are able to encapsulate and adsorb a variety of molecules, which make them appealing as DDS. Moreover, nanosponges partially overcome toxicity issues that restrict cyclodextrins from more widespread use (Allahyari et al., 2019). Recently, Femminò and colleagues (2018) proposed alpha-cyclodextrin nanosponges as a system for delivery of oxygen to infarcted tissue. In a hypoxia/reoxygenation in vitro protocol, preconditioning H9c2 myoblasts with oxygen-loaded alpha-cyclodextrin nanosponges returned cell viability to normoxic control levels (Femminò et al., 2018).
Micelle
Lipid-based micelles can passively accumulate at the infarct area with a lower latency than liposomes, and are more likely to accumulate in cardiomyocytes rather than in immune cells or vessels, even when administered one week after acute IRI (Geelen et al., 2013). In an analogous manner, polymeric micelles constituted of amphiphilic PEG and phosphatidyl-ethanolamine (PE) also concentrate at the damaged myocardium but not at the remote healthy tissue (Lukyanov et al., 2004). Moreover, to take advantage of matrix metalloproteinase (MMP) overactivity seen throughout the remodeling of the post-infarcted myocardium, Nguyen et al. (2015a) coupled lipid micelles with a MMP-targeting peptide, ensuring localization of such micelles within the remodeling heart issue. Retention of micelles was achieved by binding MMP recognition sequences to micelles in order to produce aggregates that remained up to 28 days at the remodeling heart (Nguyen et al., 2015b). Micelles can also be targeted to other cell types by changing the surface composition. This is the case of CCR antibodies that when attached to lipid micelles can decrease monocytic infiltration at the injury site (Wang et al., 2018a). Micelles allow for the solubilization of hydrophobic drugs, and as a consequence, increase their bioavailability, reduce adverse off-target effects and potentiate their ability to cross biological barriers (Musacchio and Torchilin, 2013). These characteristics make micelles a suitable DDS in the cardiovascular system. Recently, the clinically approved drug rapamycin, given chronically as a micellar nanoformulation (Rapatar), was able to reduce MI size in diabetic mice (Samidurai et al., 2017). Polymeric micelles used to deliver hydrogen sulfide donors, the release of which depends on endocytosis, produced robust protective effects on hypoxic cardiomyocytes (Takatani-Nakase et al., 2017).
Micelles have been tested for passive delivery of a variety of natural antioxidants that in their unmodified forms lack aqueous solubility. Polymeric Pluronic micelles simultaneously transporting curcumin and resveratrol lowered effector caspase activity and ROS levels in H9c2 cells treated with doxorubicin (Carlson et al., 2014). A study from the same group indicated that co-delivery of quercetin and resveratrol offered similar results in H9c2 cells, while in vivo, this combination conferred cardioprotection (Cote et al., 2015). In line with these observations, ginsenoside administered within a Pluronic micelles formulation reduced cardiac dysfunction produced by doxorubicin, presumably by safeguarding mitochondria integrity (Li et al., 2017). Another plant derivative, tilianin, a natural flavonoid, was loaded into polymeric micelles and was tested in a hypoxia-reoxygenation preparation. Either tilianin alone or entrapped in micelles significantly preserved the viability of cultured cardiomyoblasts after the simulated injury. Nonetheless, water solubility of micelles was much superior than that of the flavonoid alone (Wang et al., 2018b). In the same line, the isoflavone puerarin, embedded in PEG-PE micelles, counteracted the pro-apoptotic effects of isoprenaline in H9c2 cells. In fact, the conjugate presented a better safety profile than puerarin alone, in terms of its natural hemolytic capacity (Li et al., 2018). The addition of triphenylphosphonium cation further improved puerarin antiapoptotic efficacy, and confocal microscopy revealed that the cation drove the micelles specifically to the mitochondria (Li et al., 2019).
Hybrid Hydrogel Nanoparticles
Hydrogels are another kind of hydrophilic polymeric materials, which can work as scaffolds for cells, drugs, and other NPs (Utech and Boccaccini, 2016). For example, the hybrid system of alginate hydrogel and PLGA microspheres carrying HSP27 considerably lowered fibrosis and cell death at the infarct zone (Lee et al., 2013). Also, the composite of hydrogel and polymeric NPs carrying miRNAs represents a feasible means of cardiac restoration therapy with extended lifetime (Yang et al., 2019b). Intriguingly, a system of PLGA nanoparticle-based oxygen supply was developed and showed encouraging results as a treatment of ischemic disease. In brief, the system consisted of PLGA microspheres that released hydrogen peroxide that was rapidly converted into molecular oxygen and water by the catalase enzyme attached to a hydrogel scaffold (Fan et al., 2018). Regarding cell therapy, cardiac progenitor cells hold promise for myocardium regeneration after cardiac injury, since they are able to differentiate into cardiomyocytes, smooth muscle cells, and endothelial cells (Le and Chong, 2016). Nonetheless, retention of such cells remains a challenge. Recently, it was shown that acrylate-based, degradable, thermal and pH-sensitive hydrogels could solve this problem and make it possible for cardiosphere-derived cells to survive and differentiate at the infarct zone (Li et al., 2016).
Biomolecule-based nanoparticles
Protein-based nanoparticles
Typically, protein-based NPs are derived from water-soluble or water-insoluble proteins. Proteins have a list of properties that makes them appealing as materials for nanoparticle synthesis. Proteins are metabolizable, amphiphilic, and possess a variety of biochemical moieties for ligand binding (Lohcharoenkal et al., 2014). A particularly studied case is that of albumin. It is widely known that albumin transports both endogenous and exogenous molecules in the bloodstream because of its multiple ligand binding sites. Beyond binding, albumin guarantees an extended lifetime mostly due to renal reabsorption and endothelial recycling that keeps it circulating for up to nineteen days (Larsen et al., 2016). Associated in a non-covalent manner, a protein or peptide fused to albumin, can covalently bind ligands to one of the chemical groups exposed at its surface.
Decafluorobutane-filled albumin microbubbles infiltrate into myocardium when the heart is exposed to ultrasound, indicating the capability of these particles to be used as drug vehicles. However, ultrasound destruction of albumin microbubbles is accompanied by hemorrhage and transient left ventricle dysfunction. For these reasons, the risk of using this technique should be seriously considered (Vancraeynest et al., 2006). In a series of studies (Ji et al., 2011) investigated the feasibility of bovine serum albumin NPs linked to ultrasonic microbubbles as a gene delivery system for in vivo transfection of tissue plasminogen activator (tPA). Applying ultrasound following the injection of the aforementioned formulation resulted in targeted delivery to cardiomyocytes (Ji et al., 2011). This strategy for heart-targeted delivery of tPA based on albumin NPs was later tested in canine models of tricuspid valve replacement and coronary artery bypass grafting. In the first case, treatment with albumin NPs prevented intrachamber thrombosis and improved survival (Ji et al., 2012). In the second case, intravascular thrombosis and intimal thickening of the vein graft were potently reduced in the group treated with albumin NPs, suggesting a potential therapy for preventing coronary conduit restenosis after cardiac surgery (Ji et al., 2014). Likewise, alendronate given in an albumin nanoparticle formulation reduced the neointima/media ratio in a rat restenosis model by targeting macrophages (Markovsky et al., 2007). Another way of achieving tPA local targeting of myocardium consisted of implanting a Dacron slice coated with gelatin, which contained the tPA plasmid directly into the left atrial cavity (Liu et al., 2015).
Besides albumin, gelatin is also a promising protein material for drug delivery (Lohcharoenkal et al., 2014). In the permanent ligated hind limb, blood perfusion increased when VEGF was attached to NPs composed of glycidyl methacrylated dextran and gelatin (Xie et al., 2013). In the infarcted myocardium, co-delivery of 6-Bromoindirubin-3-oxime and IGF-1 encapsulated in gelatin NPs produced an increase in cardiomyocyte proliferation and capillary density. Importantly, this was reflected as ameliorated left ventricle functional parameters measured six weeks after surgery (Fang et al., 2015). Finally, there are some proteins with a natural tropism towards scarred myocardium. An interesting example is that of fibronectin binding domain of the Streptococcus gordonii adhesin. Recently, this motif was fused to supercharged green fluorescent protein. This chimera was bound by electrostatic forces to the plasma membrane of mesenchymal stem cells, and as a consequence these cells acquired the ability to specifically concentrate at the heart and remain there, offering hope for cell therapy (Xiao et al., 2019).
Nucleic acid-based nanoparticles
Aptamers are small single-stranded RNA/DNA oligonucleotides with the ability to recognize and bind to specific biological motifs with high affinity. In this respect, aptamers resemble antibodies, but display clear advantages over them, including lower cost of production, thermal and pH stability, low immunogenicity, and low batch-to-batch variability (Mittal et al., 2018; Tan et al., 2019). Aptamers are currently being investigated for their use as anticoagulants, anti-thrombotics and thrombolytic agents, since they are able to reversibly bind the factors implicated in the clotting cascade (Hu and Zhang, 2015). The DNA-based aptamer ARC1779 that works by binding to the A1 domain of the von Willebrand factor (vWF), demonstrated that it is capable of reducing platelet aggregation in humans (Gilbert et al., 2007). ARC1779 also effectively and safely reduced the number of embolic signals of patients that underwent carotid endarterectomy. In this context, it was suggested that it could be used as an adjunct in the treatment of myocardial ischemia (Markus et al., 2011). Amid the recent advances, the RNA-based DTRI-031 aptamer, which also targets the vWF, was shown to reestablish the blood flow of the occluded carotid arteries in both a murine and a clinically relevant canine model. DTRI-031 aptamer displayed nuclease resistance and, of note, susceptibility to be switched off by an antidote oligonucleotide. This last characteristic would strengthen the safety of aptamers in a possible clinical scenario (Nimjee et al., 2019).
Aptamers have been explored as a DDS too. In a proof of concept study, an aptamer-peptide chimera was developed. The chimera consisted of an anti-PDGFRβ aptamer and a small novel peptide (R7W-MP) with therapeutic effects on the L-type calcium channel. The chimera successfully restored the L-type calcium channel density in serum-starved HL-1 cells (Romanelli et al., 2018). Aptamers can be delivered attached to self-folding RNA origami, with the advantage of possible co-delivery of more than one aptamer. Such an approach was utilized for the delivery of two anti-thrombin aptamers, extending their life-time and reinforcing, up to seven times, their anticoagulant activity (Krissanaprasit et al., 2019). Other forms of nucleic acid-based carriers are DNA nanotubes. DNA nanotubes tailored with a pH-sensitive motif released dexamethasone at the ischemic-reperfused skeletal muscle, where the nanotubes decreased leukocyte transmigration via downregulation of vascular adhesion molecules (Sellner et al., 2017). Further experiments would unveil the efficacy of DNA nanotubes in a myocardial ischemia context.
Peptide Self-assembly
For the purpose of cardiac regeneration, self-assembling peptides are a promising option as platforms for cell growth as they can act as growth factors reservoirs. Self-assembling peptides are characterized by having predictable gelling kinetics, and biodegradability into natural amino acids. They would allow for cell recruitment, provide the biochemical signals for cell growth, and integrate without interfering with the mechanical and electrical processes of the heart (French et al., 2016). The intramyocardial injection of self-assembling peptide nanofibers along with PDGF immediately following ligation of the left coronary artery reduced MI size and increased vascular density, such that after four months of coronary ligation, regional blood flow approached normality (Hsieh et al., 2006). The fusion of a heparin-binding motif enabled self-assembling peptides for prolonged release of VEGF, such that after one month considerable amounts of VEGF could still be detected. As expected, microvascular density was also higher compared with non-treated and VEGF-only-treated animals, a phenomenon which correlated with a better contractility performance (Guo et al., 2012). Regarding cell therapy, it would be convenient for transplanted cells to encounter an optimum microenvironment for their implantation. In this regard, a self-assembling peptide scaffold with IGF-1 incorporated by means of a biotin-streptavidin bond improved the survival of transplanted cardiomyocytes (Davis et al., 2006).
3. Current Challenges and Future
Although the development of NPs as DDSs has increased in the past decade, NPs with multi-functions have mainly been applied in the field of cancer research. In clinical trials, using therapeutic NPs in a treatment regimen is rarely used as a first line treatment, but are only available to patients as a last resort, when they have stopped responding to other treatments (Satalkar et al., 2016). Also, limited cases have been successfully translated into clinical settings to treat other diseases besides cancer. In this section, we discuss some of the challenges facing NPs delivery systems in CVD and cardioprotection (Ho et al., 2016).
3.1. Biological Challenges
As the main organ and critical pump in the body, the heart is sensitive and very resistant to foreign objects. This makes delivering drugs into the heart muscle more challenging. In most cases, biodistribution in the heart after administration of nanomedicine is minimal. In acute myocardial IRI, the coronary microvasculature becomes leaky, a well-known phenomenon in tumors, termed the enhanced permeability and retention (EPR) effect (Weis, 2008). The EPR effect makes it possible for NPs to deliver therapeutics into the ischemic heart. Another challenge is from the immune system, which is easy to be stimulated by foreign injection with NPs resulting in fast clearance from the blood. To allow the NPs to remain in the body for a longer time and to avoid being removed by immune cells, NPs can be PEGylated or PEG-terminated. Similarly, using hydrophilic sugar like dextran to coat iron-oxide NPs bring about the same effect. Another way to extend the half-life before immune recognition is decorating biological proteins, like albumin. In term of acute myocardial IRI, there is a special need to protect the NPs in the acute phase when most IR injury occurs. This sets a critical requirement for DDSs to accumulate in the heart rapidly and efficiently.
Yet another challenge comes from the intrinsic complexity of IRI pathophysiology. Since multiple independent pathways are known to contribute to the pathophysiology of IRI, it is important to stress the need for a multi-target approach to cardioprotection (Rossello and Yellon, 2018). From a therapeutic standpoint, NPs could be loaded with a combination of multi-target cargoes intended to combat IRI. In this manner, additive cardioprotection can be achieved by targeting two or more signaling pathways or the same pathway at different points, or even several cell types, including cardiomyocytes, endothelial cells, platelets, macrophages, and fibroblasts (Davidson et al., 2019).
3.2. Toxicity Challenges
Concern over patient safety is one of the main issues impeding the translation of nanomedicine into clinical practice. As a new type of therapy, toxicity studies of nanomedicine have been commonly neglected in the past decades. Despite an increasing interest in safety aspects of various nanomaterials, there is currently no standard to evaluate and categorize their toxic levels. As such, a systematic toxicity protocol should be standardized. The application in the heart requires special attention to cellular toxicity and to the biological fate of the materials, especially when salvaging cells is the target in cardioprotection. Using FDA-proven and biodegradable materials to constructing NPs is a strategy for translational nanomedicine. Physical clearance must be investigated in those non-degradable materials such as inorganic NPs for cardiac application.
3.3. Technological Challenges
Technological challenges of NPs in the lab include scale-up synthesis, performance optimization, and performance predictions. In preclinical studies, NPs are synthesized in small batches, and it is not always possible to scale up for large quantity synthesis. For performance optimization, nanoparticle formulations that provide the best results in animal models have the most potential in clinical trials, but these are not systematically optimized. Correlation between animal and human data is essential for predictions, as there are many differences and similarities between them. Thus, this poses a challenge for predicting nanoparticle performance at the preclinical and clinical level. Efforts to correlate the results should be implemented as soon as possible to determine any general trends, if possible, to allow for better results. There are also difficulties in analyzing and determining the effectiveness of the nanomedicine in humans, as most quantitative techniques require organ isolation or tissue harvesting. Non-invasive imaging techniques may be a solution in studying time-dependent biodistribution. However, imaging the beating heart with spatial resolution is still challenging.
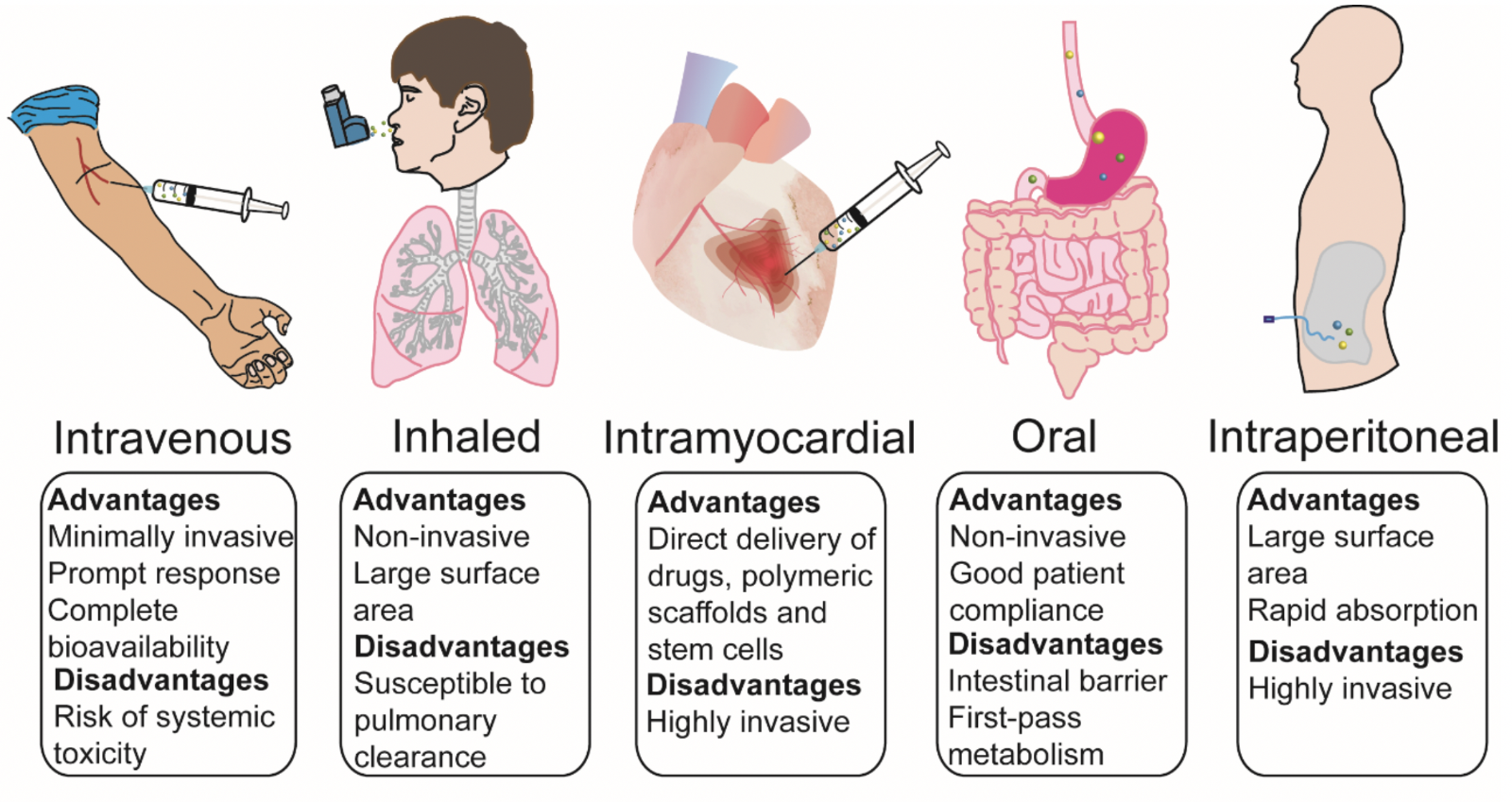
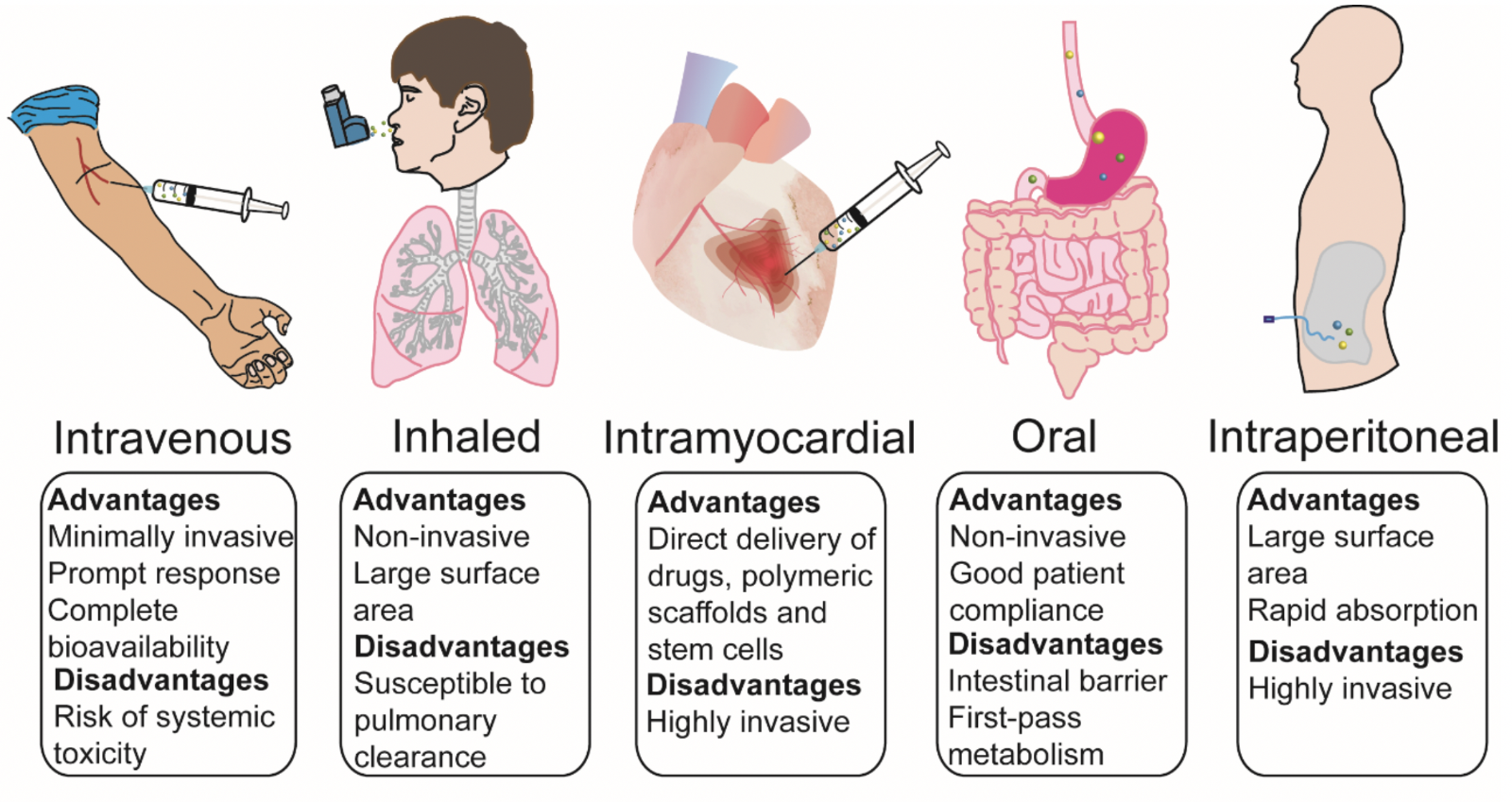
3.4. Administration Routes
Intravenous injection has been the main route used for administration of NPs intended as treatment of AMI. To achieve more specific local delivery, in the case of hydrogels and self-assembling peptides, intramyocardial injection is preferred with proper retention. However, this invasive route has limited clinical availability and has a higher risk. Other routes for cardiac delivery of NPs have been explored, including oral (Simoń-Yarza et al., 2013), inhalation (Miragoli et al., 2018) and intraperitoneal injection (Abdelhalim, 2011), as potential alternatives to the intravenous route. Further investigations are needed to verify whether these routes are suitable in other type of NPs in AMI treatment. Overall, the advantages and disadvantages of each route are briefly summarized in Figure 3.
In a new window | Download PPT
Figure 3: Potential routes of nanoparticle administration applied in cardiovascular disease - advantages/disadvantages.
4. Conclusions
Over recent years nanomedicine has been used to increase the bioavailability and delivery of therapies to treat CVD, including acute myocardial IRI. NPs, which hold promise as DDS, are liposomes, polymeric NPs, and micelles, and of these, PLGAs and liposomes are already FDA approved for use in clinical trials. The advances in NPs make their application promising in term of delivering diagnosis and targeting therapeutics to the ischemic heart following AMI. There are challenges in translating nanomedicine into the clinic, and these are primarily concerns related to safety. To overcome these challenges, further investigation of NP design in relation to both safety and efficacy are essential for the future of translational nanomedicine in CVD and cardioprotection.
Conflicts of interest statement
The authors declare that they have no conflicts of interest.
Acknowledgements:
William Boisvert was supported by grant U54 MD007601 from the NIH. Shengjie Lu was supported by the Singapore Ministry of Health’s National Medical Research Council under Open Fund–Young Individual Research Grant (OF-YIRG)–MOH-000230, Academic Medicine Research Grant- AM/TP014/2018 (SRDUKAMR1811) from SingHealth Duke-NUS Academic Medicine Centre, as well as a Khoo Postdoctoral Fellowship Award (KPFA) – DUKE-NUS-KPFA/2018/0026 from the Estate of Tan Sri Khoo Teck Puat, Singapore. Derek Hausenloy was supported by the British Heart Foundation (CS/14/3/31002), the National Institute for Health Research University College London Hospitals Biomedical Research Centre, Duke-National University Singapore Medical School, Singapore Ministry of Health’s National Medical Research Council under its Clinician Scientist-Senior Investigator scheme (NMRC/CSA-SI/0011/2017) and Collaborative Centre Grant scheme (NMRC/CGAug16C006), and the Singapore Ministry of Education Academic Research Fund Tier 2 (MOE2016-T2-2-021). This article is based upon work from COST Action EU-CARDIOPROTECTION CA16225 supported by COST (European Cooperation in Science and Technology). HA Cabrera-Fuentes was supported by the Russian Government Program for competitive growth of Kazan Federal University, Kazan (Russian Federation), by the Singapore Heart Foundation (SHF/FG657P/2017), and by the von Behring-Röntgen-Foundation (Marburg, Germany).
References
Abraham Mendez-Fernandez1,2
1Tecnologico de Monterrey, Centro de Biotecnologia-FEMSA, Nuevo Leon, Mexico. 2National Heart Research Institute Singapore, National Heart Centre, Singapore.
Hector A. Cabrera-Fuentes1-6
1Tecnologico de Monterrey, Centro de Biotecnologia-FEMSA, Nuevo Leon, Mexico. 2National Heart Research Institute Singapore, National Heart Centre, Singapore. 3SingHealth Duke-NUS Cardiovascular Sciences Academic Clinical Programme, Duke-National University of Singapore Medical School, Singapore. 4Cardiovascular and Metabolic Disorders Program, Duke-National University of Singapore Medical School, Singapore. 5Institute of Fundamental Medicine and Biology, Kazan (Volga Region) Federal University, Russian Federation. 6Institute of Physiology, Medical School, Justus-Liebig-University, Germany.
Bhaarathy Velmurugan2,4
2National Heart Research Institute Singapore, National Heart Centre, Singapore. 4Cardiovascular and Metabolic Disorders Program, Duke-National University of Singapore Medical School, Singapore.
Jason Irei7
7Center for Cardiovascular Research, John A. Burns School of Medicine, University of Hawaii, USA.
William A. Boisvert7
7Center for Cardiovascular Research, John A. Burns School of Medicine, University of Hawaii, USA.
Shengjie Lu2,3
2National Heart Research Institute Singapore, National Heart Centre, Singapore. 3SingHealth Duke-NUS Cardiovascular Sciences Academic Clinical Programme, Duke-National University of Singapore Medical School, Singapore.
Derek J. Hausenloy2,4,8,9,10
2National Heart Research Institute Singapore, National Heart Centre, Singapore. 4Cardiovascular and Metabolic Disorders Program, Duke-National University of Singapore Medical School, Singapore. 8The Hatter Cardiovascular Institute, Institute of Cardiovascular Science, University College London, UK. 9Yong Loo Lin School of Medicine, National University Singapore, Singapore. 10Cardiovascular Research Center, College of Medical and Health Sciences, Asia University, Taiwan.
Corresponding author:
Professor Derek Hausenloy
Email: derek.hausenloy@duke-nus.edu.sg
or
Shengjie Lu
Email: lushengjie10@gmail.com
In a new window | Download PPT
Figure 1: Schematic illustration of nanoparticle delivery in acute myocardial infarction.
In a new window | Download PPT
Figure 2: Schematic structure of various nanoparticles that have been applied as drug delivery systems in cardiovascular disease and cardioprotection.
In a new window | Download PPT
Figure 3: Potential routes of nanoparticle administration applied in cardiovascular disease - advantages/disadvantages.
Supporting Information
Metrics
| Full-Text | Supporting Information | ||
|---|---|---|---|
| Number | 12551 | 49 | 0 |
Copyright © 2017 Conditioning Medicine, All Rights Reserved.
Address: Conditioning Medicine Editorial Office, 3500 Terrace Street, Pittsburgh, PA, 15213, USA